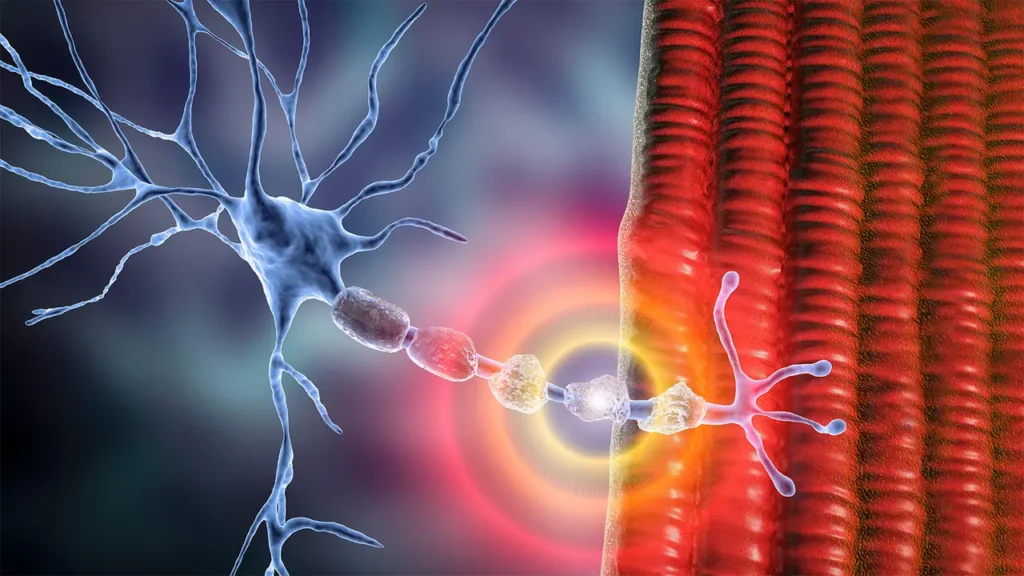
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare, acquired disorder that affects the peripheral nervous system. It primarily involves the demyelination of nerves, leading to motor and sensory dysfunction. CIDP is often characterized by progressive muscle weakness, sensory loss, and reflex changes. As an autoimmune condition, CIDP is caused by the body’s immune system mistakenly attacking the myelin sheath that protects nerve fibers, resulting in impaired nerve signaling. Early detection and treatment are crucial in preventing further damage and improving the quality of life for those affected.
Understanding CIDP: What Is Chronic Inflammatory Demyelinating Polyneuropathy?
CIDP is a form of polyneuropathy, meaning it affects multiple peripheral nerves. The condition primarily targets the myelin sheath—the fatty covering that insulates nerve fibers and ensures efficient transmission of electrical signals. The demyelination process, in which the immune system attacks and damages this protective layer, leads to a slower or disrupted nerve signal transmission, causing muscle weakness, numbness, and other neurological symptoms.
CIDP can develop gradually or in episodes, and its severity can range from mild to disabling. The condition is more commonly diagnosed in adults, although it can occur at any age.
Causes of Chronic Inflammatory Demyelinating Polyneuropathy
CIDP is generally considered an autoimmune disorder, where the immune system turns against the body’s own tissues. The exact cause of this immune system dysfunction is not always clear, but several factors are believed to contribute to its development:
- Genetic Predisposition: Certain genetic factors may make individuals more susceptible to CIDP. Although it is not inherited in a simple manner, familial cases have been reported.
- Infections: Some viral and bacterial infections are believed to trigger the onset of CIDP by provoking an immune response that mistakenly attacks the nervous system.
- Vaccinations: In rare cases, vaccinations have been linked to CIDP, although this connection remains controversial and under study.
- Underlying Health Conditions: Conditions such as diabetes, HIV, and certain cancers may increase the risk of developing CIDP.
Key Symptoms of CIDP
The symptoms of CIDP typically develop gradually over time, although in some cases, they can appear suddenly or in episodes. The most common symptoms include:
- Muscle Weakness: Particularly in the arms, legs, and face, muscle weakness is one of the hallmark symptoms of CIDP.
- Numbness and Tingling: Individuals with CIDP may experience sensations of numbness, tingling, or a “pins and needles” feeling in the limbs.
- Impaired Reflexes: Reduced or absent reflexes, such as the knee-jerk reflex, are frequently observed in people with CIDP.
- Pain: Some individuals report experiencing nerve pain or aching sensations in the affected areas.
- Fatigue: Chronic fatigue and generalized weakness are often present in CIDP, making daily activities challenging.
- Loss of Coordination: Difficulty walking or maintaining balance can occur as a result of muscle weakness and sensory changes.
Diagnosing CIDP
Early and accurate diagnosis of CIDP is essential for effective treatment and management. The diagnostic process typically involves the following:
- Clinical Evaluation: A detailed medical history and physical examination are crucial in identifying symptoms indicative of CIDP. The doctor will assess muscle strength, reflexes, and sensory function.
- Electrodiagnostic Studies: Nerve conduction studies (NCS) and electromyography (EMG) help assess the electrical activity in nerves and muscles. These tests can reveal slowed nerve conduction velocities, a key sign of demyelination.
- Cerebrospinal Fluid (CSF) Analysis: Elevated protein levels in the CSF, without an increase in white blood cells, are indicative of CIDP.
- Nerve Biopsy: In rare cases, a nerve biopsy may be performed to assess the extent of nerve damage.
CIDP Treatment Options
There is no cure for CIDP, but a variety of treatment options are available to manage symptoms and slow disease progression. The goal of treatment is to reduce inflammation, prevent further nerve damage, and improve motor function. Common treatment strategies include:
1. Immunosuppressive Therapy
Since CIDP is an autoimmune disorder, treatments that suppress the immune system are often effective. These include:
- Corticosteroids: Drugs like prednisone are commonly used to reduce inflammation and control symptoms. However, long-term use can have significant side effects.
- Plasmapheresis: This treatment involves removing antibodies from the blood to reduce immune system activity. It is typically used for patients with severe symptoms.
- Intravenous Immunoglobulin (IVIG): IVIG treatment involves infusing immunoglobulins (antibodies) from donated blood to help regulate the immune system and reduce inflammation.
2. Physical Therapy
Physical therapy plays an essential role in CIDP management. It helps to maintain muscle strength, prevent joint contractures, and improve coordination. A tailored exercise program can significantly improve mobility and independence.
3. Pain Management
Managing pain is another key aspect of CIDP treatment. Depending on the severity, patients may be prescribed pain-relieving medications, including analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), or neuropathic pain medications like gabapentin.
4. Surgical Intervention
In some cases, patients may require surgery to address complications arising from muscle weakness, such as joint deformities or nerve compression.
Prognosis and Living with CIDP
The prognosis for individuals with CIDP varies depending on the severity of the disease, the speed of diagnosis, and the response to treatment. With early intervention and appropriate therapy, many people with CIDP can manage their symptoms and lead relatively normal lives. However, without treatment, CIDP can lead to permanent nerve damage and disability.
It is important for individuals with CIDP to work closely with their healthcare providers to monitor the condition and adjust treatment plans as needed. Psychological support, through counseling or support groups, may also help patients cope with the challenges associated with living with a chronic illness.
CIDP and Lifestyle Modifications
While CIDP can significantly impact daily life, making certain lifestyle modifications can help individuals manage their condition more effectively. These include:
- Nutrition: A balanced diet rich in vitamins and minerals, particularly B vitamins and antioxidants, can help maintain nerve health.
- Stress Management: Reducing stress through relaxation techniques, such as meditation or yoga, can help reduce flare-ups of symptoms.
- Regular Exercise: Engaging in low-impact exercises, such as swimming or walking, can help maintain muscle strength and prevent deconditioning.