Chronic hepatitis C, caused by the hepatitis C virus (HCV), remains a significant global health concern. Among the six primary genotypes of HCV, genotype 2 is less prevalent but notable for its generally favorable response to treatment. This article delves into the essential aspects of chronic hepatitis C genotype 2, encompassing symptoms, diagnosis, treatment modalities, and long-term management strategies.
Epidemiology and Prevalence of Genotype 2
HCV genotype 2 is responsible for a smaller percentage of global hepatitis C cases, with higher prevalence in specific regions such as West Africa and parts of East Asia. Its comparatively lower global prevalence underscores the importance of targeted public health measures in regions where it is endemic.
Symptoms and Disease Progression
Early-Stage Symptoms
- Fatigue: A common early indicator of chronic hepatitis C.
- Mild abdominal discomfort: Particularly in the upper-right quadrant, signaling liver involvement.
- Joint pain and nausea: General systemic symptoms of HCV infection.
Advanced-Stage Symptoms
If untreated, genotype 2 can lead to more severe liver complications:
- Jaundice: Yellowing of the skin and eyes due to elevated bilirubin levels.
- Ascites: Fluid accumulation in the abdominal cavity.
- Hepatic encephalopathy: Cognitive impairments stemming from liver dysfunction.
Diagnosis of HCV Genotype 2
Accurate diagnosis is essential for initiating effective treatment. The process includes:
- Serological Testing: Detects anti-HCV antibodies.
- RNA Testing: Confirms active HCV infection and quantifies viral load.
- Genotyping: Determines the specific genotype of the virus, which guides treatment planning.
- Liver Function Tests (LFTs): Assesses liver damage through enzymes such as ALT and AST.
- Fibrosis Assessment:
- Transient elastography (FibroScan): Measures liver stiffness.
- Biopsy: Rarely performed but provides detailed information on liver damage.
Treatment Strategies for Genotype 2
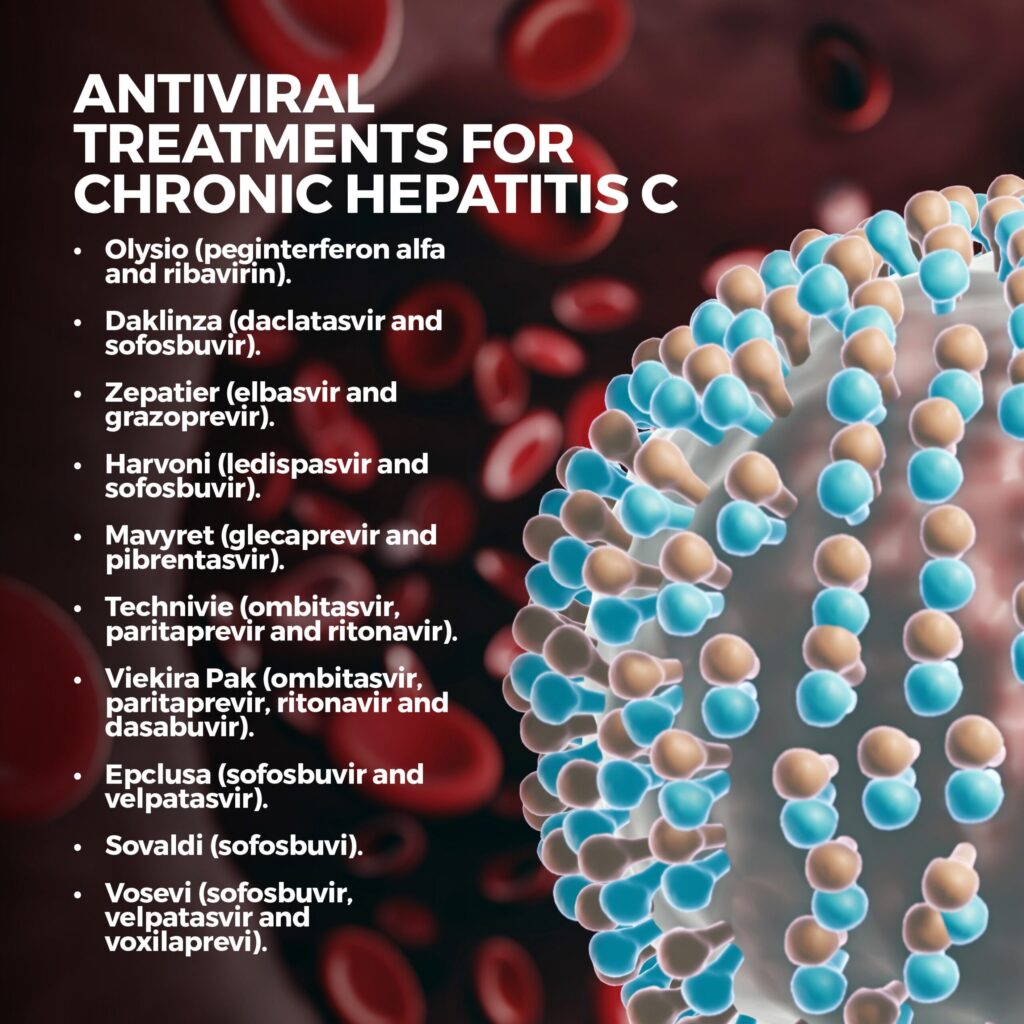
Antiviral Therapies
HCV genotype 2 typically responds well to direct-acting antivirals (DAAs). Standard regimens include:
- Sofosbuvir and Ribavirin: A combination therapy often prescribed for 12 weeks. This regimen boasts a high sustained virologic response (SVR) rate exceeding 95%.
- Pangenotypic DAAs: Such as glecaprevir-pibrentasvir, effective across all HCV genotypes and particularly beneficial for patients with co-infections or comorbidities.
Key Factors Influencing Treatment Success
- Adherence to therapy: Crucial for achieving SVR.
- Baseline viral load: Higher loads may necessitate extended treatment duration.
- Liver fibrosis stage: Advanced fibrosis or cirrhosis may require tailored treatment protocols.
Long-Term Management and Complications
Monitoring Post-Treatment
Even after achieving SVR, ongoing monitoring is essential to ensure liver health. Recommendations include:
- Regular LFTs: To assess liver function.
- Ultrasound Screening: Annual imaging for early detection of hepatocellular carcinoma (HCC) in patients with advanced fibrosis.
Managing Comorbidities
Chronic hepatitis C often coexists with conditions such as diabetes, metabolic syndrome, and cardiovascular disease. Addressing these comorbidities enhances overall patient outcomes.
Lifestyle Modifications
- Alcohol Avoidance: Reduces further liver damage.
- Balanced Diet: Supports liver regeneration and overall health.
- Regular Exercise: Improves metabolic health and reduces liver fat accumulation.
Prognosis for Genotype 2 Patients
With advancements in DAA therapies, the prognosis for individuals with HCV genotype 2 has significantly improved. Achieving SVR greatly reduces the risk of liver-related complications and enhances quality of life. Early diagnosis and adherence to treatment are critical for optimal outcomes.