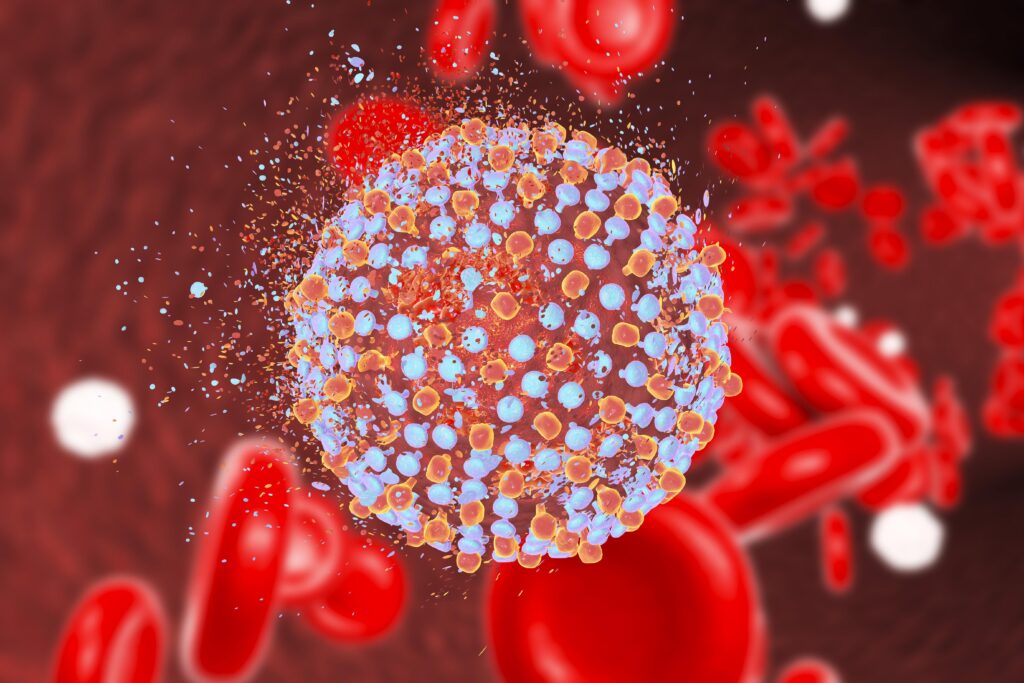
Hepatitis C, caused by the hepatitis C virus (HCV), remains a significant global health challenge. Among its six major genotypes, genotype 1 is the most prevalent worldwide, accounting for a substantial proportion of chronic infections. This article explores the intricacies of chronic hepatitis C genotype 1, from its epidemiology and clinical manifestations to advanced therapeutic options.
Epidemiology of Genotype 1 Hepatitis C
Genotype 1 is the most common form of HCV in regions such as North America, Europe, and parts of Asia. It is further divided into subtypes 1a and 1b, with notable geographical differences:
- Subtype 1a: Predominant in North America and northern Europe.
- Subtype 1b: Common in Japan and central Europe, often linked to older age groups and previous blood transfusions.
Risk Factors
Chronic hepatitis C genotype 1 shares risk factors with other HCV genotypes, including:
- Intravenous drug use.
- Blood transfusions before 1992 (prior to rigorous screening measures).
- Needle-stick injuries in healthcare settings.
- Vertical transmission from mother to child.
- High-risk sexual practices.
Clinical Manifestations
Many individuals with genotype 1 HCV remain asymptomatic for years. However, without timely diagnosis and treatment, chronic infection can lead to serious complications:
- Acute phase: Mild or nonspecific symptoms such as fatigue, nausea, and jaundice.
- Chronic phase: Progressive liver damage, often culminating in:
- Fibrosis: Scarring of liver tissue.
- Cirrhosis: Advanced liver scarring with potential for liver failure.
- Hepatocellular carcinoma (HCC): Increased risk of liver cancer.
Extrahepatic Manifestations
Genotype 1 HCV is also associated with extrahepatic conditions such as:
- Cryoglobulinemia.
- Insulin resistance and type 2 diabetes.
- Lymphoproliferative disorders.
- Chronic fatigue syndrome.
Diagnostic Approach
Accurate diagnosis is critical for effective management. Diagnostic steps include:
- Serological Testing:
- Detection of anti-HCV antibodies.
- Confirmation of active infection with HCV RNA testing.
- Genotype Testing:
- Determines the specific genotype and subtype for tailored therapy.
- Liver Assessment:
- Non-invasive imaging techniques (e.g., elastography).
- Biopsy in select cases to evaluate the extent of liver damage.
Treatment Options for Genotype 1
The advent of direct-acting antivirals (DAAs) has revolutionized HCV treatment, offering high cure rates with fewer side effects compared to older interferon-based regimens. Key considerations for genotype 1 treatment include:
Standard of Care
- DAA Combinations: Regimens often include sofosbuvir combined with agents like ledipasvir, velpatasvir, or glecaprevir/pibrentasvir.
- Treatment Duration: Typically 8-12 weeks, depending on the presence of cirrhosis or prior treatment history.
- Sustained Virologic Response (SVR): Achieved in over 95% of cases, indicating viral eradication.
Addressing Special Populations
- Cirrhotic Patients: May require extended treatment durations or intensified monitoring.
- Renal Impairment: Adjustments are necessary to avoid nephrotoxic effects.
- Post-Transplant Recurrence: Careful selection of DAAs is essential to prevent graft dysfunction.
Advances in Therapeutics
Recent research continues to enhance our understanding of genotype 1 HCV treatment. Promising developments include:
- Pan-Genotypic Regimens: Effective across all genotypes, simplifying treatment algorithms.
- Resistance-Associated Substitutions (RASs): Improved diagnostics help optimize therapy in patients with drug-resistant variants.
- Emerging Antiviral Agents: Ongoing trials focus on shorter treatment durations and novel drug combinations.
Prevention Strategies
Preventing new infections is as crucial as treating existing cases. Key prevention measures include:
- Screening: Routine testing for high-risk populations.
- Harm Reduction: Needle exchange programs and safe injection practices.
- Education: Awareness campaigns targeting at-risk communities.
- Vaccination Research: Although no HCV vaccine exists, efforts continue to develop one.
Prognosis
With effective treatment, the long-term prognosis for individuals with genotype 1 HCV has dramatically improved. Achieving SVR significantly reduces the risk of complications such as cirrhosis and HCC, underscoring the importance of early diagnosis and intervention.