Chronic heart failure following myocardial infarction is a progressive condition characterized by the heart’s inability to pump blood efficiently to meet the body’s metabolic needs. Myocardial infarction (MI), commonly referred to as a heart attack, often serves as a precursor to CHF. The damage caused by MI leads to structural and functional changes in the heart, significantly increasing the risk of heart failure.
Pathophysiology: How Myocardial Infarction Leads to CHF
Initial Damage from Myocardial Infarction
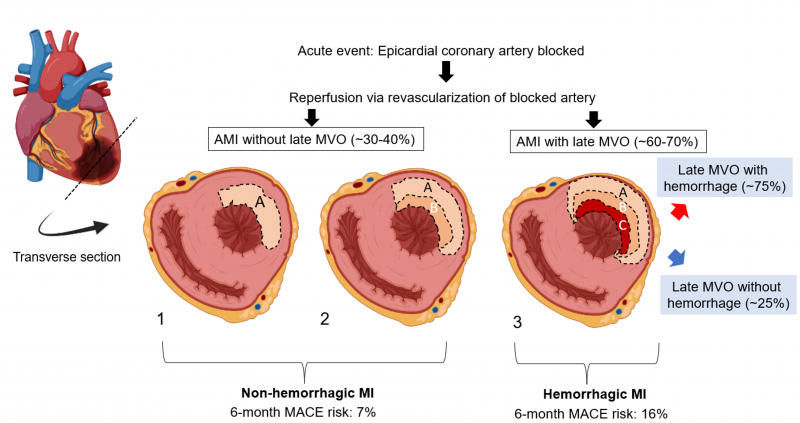
When a myocardial infarction occurs, blood flow to a portion of the heart is blocked, leading to ischemia and necrosis of myocardial tissue. The extent of damage depends on factors such as the duration of ischemia and the size of the affected artery.
Remodeling and Left Ventricular Dysfunction
Post-MI, the heart undergoes a process known as remodeling. This includes:
- Ventricular dilation: Expansion of the left ventricle to compensate for lost contractile function.
- Myocardial fibrosis: Replacement of necrotic tissue with fibrous scar tissue, reducing elasticity.
- Hypertrophy: Thickening of myocardial walls as a compensatory mechanism.
These changes result in left ventricular dysfunction, which is a hallmark of CHF.
Neurohormonal Activation
The renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system (SNS) are activated following MI, aiming to maintain cardiac output. Over time, however, these systems exacerbate heart failure by increasing vascular resistance, fluid retention, and myocardial stress.
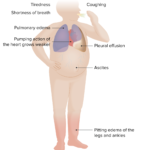
Symptoms of Chronic Heart Failure Post-MI
Patients with CHF following MI may present with a variety of symptoms, including:
- Dyspnea: Difficulty breathing, especially during physical activity or while lying down.
- Fatigue: Persistent tiredness due to inadequate blood flow.
- Edema: Swelling in the lower extremities caused by fluid retention.
- Orthopnea: Shortness of breath when lying flat.
- Reduced Exercise Tolerance: Difficulty performing physical activities due to poor cardiac output.
Diagnostic Tools for CHF Following MI
Imaging Techniques
- Echocardiography: Assesses left ventricular ejection fraction (LVEF) and identifies structural abnormalities.
- Cardiac MRI: Provides detailed imaging to evaluate scar tissue and myocardial viability.
- Chest X-ray: Detects pulmonary congestion and cardiomegaly.
Biomarkers
- B-type Natriuretic Peptide (BNP) and N-terminal proBNP (NT-proBNP): Elevated levels indicate heart failure.
- Troponin Levels: Help assess ongoing myocardial damage.
Stress Testing
Exercise or pharmacological stress tests evaluate the heart’s response under strain and can reveal functional impairments.
Treatment Strategies for CHF Post-MI
Pharmacological Interventions
- Angiotensin-Converting Enzyme (ACE) Inhibitors: Reduce afterload and prevent remodeling.
- Beta-Blockers: Lower myocardial oxygen demand and improve survival.
- Mineralocorticoid Receptor Antagonists (MRAs): Decrease fluid retention and improve cardiac function.
- Diuretics: Alleviate symptoms of fluid overload such as edema.
- SGLT2 Inhibitors: Emerging as beneficial in heart failure management, even in non-diabetic patients.
Device-Based Therapies
- Implantable Cardioverter Defibrillators (ICDs): Prevent sudden cardiac death in patients with reduced LVEF.
- Cardiac Resynchronization Therapy (CRT): Improves ventricular synchronization and cardiac efficiency.
Lifestyle Modifications
- Dietary Changes: Low-sodium and heart-healthy diets.
- Physical Activity: Tailored exercise regimens under medical supervision.
- Smoking Cessation: Reduces cardiovascular risk.
- Weight Management: Helps reduce strain on the heart.
Prognosis and Long-Term Management
The prognosis of CHF following MI varies based on factors such as the extent of myocardial damage, adherence to treatment, and comorbid conditions. Long-term management focuses on reducing symptoms, preventing disease progression, and improving quality of life.
Preventive Measures
Early Intervention
Prompt treatment during an MI, including reperfusion strategies like percutaneous coronary intervention (PCI) or thrombolysis, minimizes myocardial damage and lowers the risk of CHF.
Risk Factor Management
- Hypertension Control: Maintain blood pressure within target ranges.
- Diabetes Management: Tight glycemic control to prevent vascular complications.
- Lipid Management: Statins to reduce cholesterol levels.