What is Chronic Heart Failure?
Chronic heart failure (CHF) is a persistent condition where the heart is unable to pump blood effectively to meet the body’s needs. This results in inadequate oxygen and nutrient delivery to tissues, leading to various systemic complications. CHF is a progressive disorder that typically develops over time, requiring ongoing management and treatment to improve quality of life and prevent worsening symptoms.
Causes of Chronic Heart Failure
The causes of chronic heart failure are often multifactorial, with the most common being:
- Coronary Artery Disease (CAD): Blockages in the coronary arteries reduce blood flow to the heart muscle, leading to ischemia and weakened heart function.
- Hypertension: Persistent high blood pressure forces the heart to work harder, which can eventually lead to heart muscle weakening.
- Cardiomyopathy: Diseases of the heart muscle, such as dilated or hypertrophic cardiomyopathy, impair the heart’s ability to pump efficiently.
- Valvular Heart Disease: Dysfunction of the heart valves disrupts normal blood flow, putting added strain on the heart.
- Myocardial Infarction: Heart attacks cause damage to the heart muscle, reducing its pumping capacity.
- Congenital Heart Defects: Structural abnormalities present at birth can lead to CHF over time.
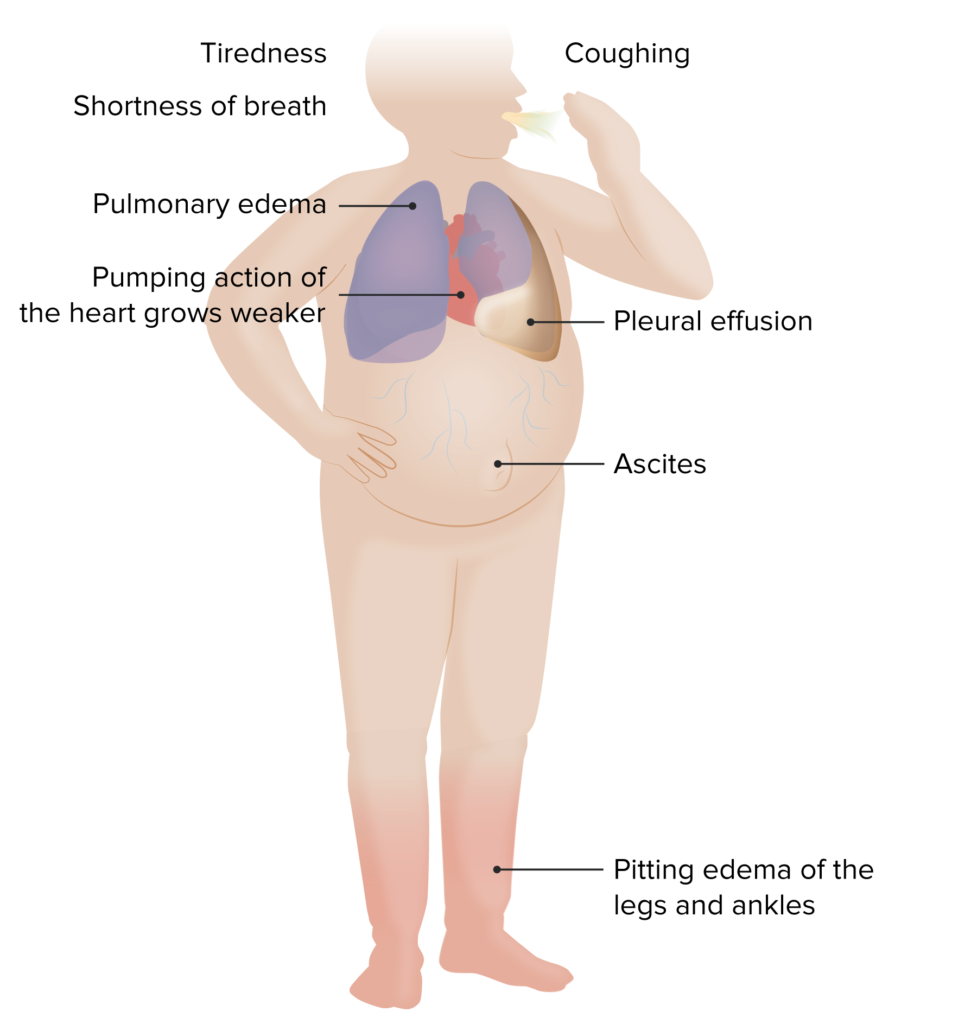
Symptoms of Chronic Heart Failure
Common symptoms of CHF include:
- Shortness of breath (dyspnea), especially during exertion or while lying flat.
- Fatigue and weakness.
- Swelling (edema) in the legs, ankles, and feet.
- Rapid or irregular heartbeat (arrhythmias).
- Persistent cough or wheezing, often with white or pink-tinged phlegm.
- Difficulty concentrating or decreased alertness.
- Sudden weight gain from fluid retention.
Pathophysiology of Chronic Heart Failure
Chronic heart failure can be classified into two main types based on the underlying mechanism:
- Heart Failure with Reduced Ejection Fraction (HFrEF): The left ventricle becomes weakened and cannot pump blood effectively.
- Heart Failure with Preserved Ejection Fraction (HFpEF): The left ventricle maintains normal pumping ability but becomes stiff and less compliant, limiting blood filling during diastole.
Diagnosis of Chronic Heart Failure
Accurate diagnosis of CHF requires a combination of clinical evaluation, imaging, and laboratory tests:
- Physical Examination: Assessment of symptoms, heart sounds, and fluid retention.
- Electrocardiogram (ECG): Detects arrhythmias or evidence of prior myocardial infarction.
- Echocardiogram: Evaluates heart structure and function, including ejection fraction.
- Chest X-Ray: Identifies fluid buildup in the lungs or heart enlargement.
- Blood Tests: Measures biomarkers like B-type natriuretic peptide (BNP) and troponins.
- Stress Tests: Assesses heart function under physical exertion or pharmacological stimulation.
Treatment of Chronic Heart Failure
The management of CHF involves lifestyle changes, medications, and advanced interventions:
Lifestyle Modifications
- Dietary Changes: Low-sodium diet to reduce fluid retention and control blood pressure.
- Regular Exercise: Tailored exercise programs to improve cardiovascular fitness.
- Smoking Cessation: Reduces strain on the cardiovascular system.
- Fluid Restriction: Helps prevent fluid overload.
Medications
- ACE Inhibitors or ARBs: Reduce blood pressure and heart workload.
- Beta-Blockers: Slow heart rate and improve pumping efficiency.
- Diuretics: Help remove excess fluid to alleviate symptoms.
- Aldosterone Antagonists: Prevent fluid retention and fibrosis.
- SGLT2 Inhibitors: Emerging therapy for improving outcomes in CHF patients.
Advanced Therapies
- Implantable Devices: Pacemakers and implantable cardioverter-defibrillators (ICDs) for rhythm management.
- Left Ventricular Assist Devices (LVADs): Mechanical pumps to support heart function.
- Heart Transplantation: Considered for end-stage CHF patients.
Complications of Chronic Heart Failure
Untreated or poorly managed CHF can lead to serious complications, including:
- Pulmonary edema (fluid accumulation in the lungs).
- Kidney dysfunction.
- Arrhythmias (e.g., atrial fibrillation).
- Stroke or other thromboembolic events.
- Worsening heart failure leading to cardiogenic shock.
Prevention
Preventing CHF involves addressing risk factors and maintaining overall cardiovascular health:
- Manage Hypertension: Keep blood pressure within a healthy range.
- Control Diabetes: Optimize blood sugar levels to reduce vascular damage.
- Adopt a Heart-Healthy Lifestyle: Balanced diet, regular exercise, and smoking cessation.
- Regular Health Screenings: Early detection and treatment of heart-related conditions.