Chronic eosinophilic leukemia (CEL) is a rare and complex form of leukemia that primarily involves an abnormal increase in eosinophils, a type of white blood cell responsible for immune responses, especially in combating parasitic infections and allergic reactions. Although it shares characteristics with other forms of leukemia, CEL presents unique challenges in diagnosis, treatment, and management. This article provides a comprehensive overview of chronic eosinophilic leukemia, shedding light on its pathophysiology, symptoms, diagnosis, treatment options, and prognosis.
What is Chronic Eosinophilic Leukemia?
Chronic eosinophilic leukemia is a hematologic disorder characterized by the uncontrolled proliferation of eosinophils in the bone marrow and peripheral blood. Eosinophils are typically involved in inflammatory responses and are crucial in the body’s defense against parasitic infections and allergic diseases. However, in CEL, these cells become abnormally elevated, leading to a range of symptoms and complications that affect multiple organs.
Pathophysiology of Chronic Eosinophilic Leukemia
The pathophysiology of CEL remains a subject of ongoing research, but it is believed to arise from mutations in the hematopoietic stem cells. These mutations result in the abnormal growth and differentiation of eosinophils. Over time, this excess of eosinophils can accumulate in various tissues and organs, such as the skin, lungs, gastrointestinal system, and heart, leading to organ dysfunction. Genetic mutations and chromosomal abnormalities, including rearrangements of the FIP1L1-PDGFRα gene, are commonly observed in patients with CEL.
Symptoms of Chronic Eosinophilic Leukemia
The symptoms of chronic eosinophilic leukemia can vary greatly from one patient to another, largely depending on the extent of eosinophil proliferation and organ involvement. Common symptoms include:
- Fatigue: Chronic fatigue is one of the most common complaints among CEL patients, often resulting from anemia or the body’s effort to manage the high eosinophil levels.
- Fever: Persistent or recurrent fevers may occur as a result of the underlying hematologic condition.
- Weight Loss: Unexplained weight loss can be a sign of the disease, often due to increased metabolic activity and the body’s response to inflammation.
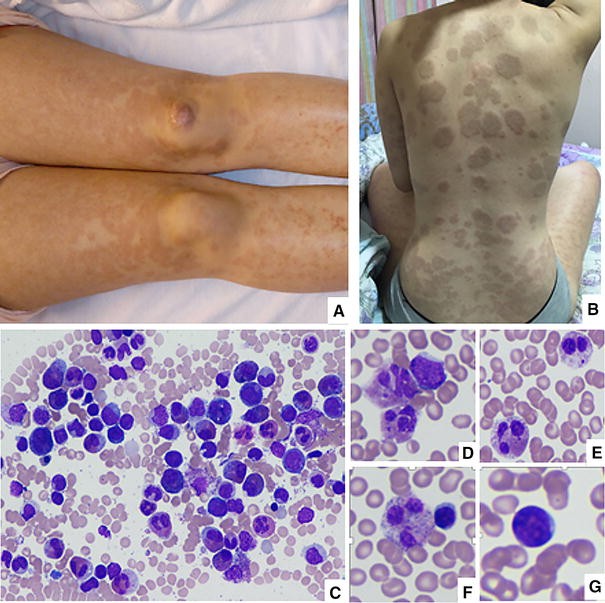
- Eosinophilic Infiltration: A buildup of eosinophils in various organs can lead to specific symptoms, such as skin rashes, gastrointestinal issues (such as diarrhea and abdominal pain), and respiratory problems, including asthma-like symptoms.
- Enlarged Spleen and Liver: Organomegaly (enlargement of the spleen and liver) is often observed, leading to discomfort and potential dysfunction of these organs.
- Peripheral Neuropathy: In some cases, CEL can result in nerve damage, causing numbness, tingling, and pain in the extremities.
Diagnosis of Chronic Eosinophilic Leukemia
Diagnosing chronic eosinophilic leukemia involves a combination of clinical evaluation, laboratory tests, and genetic analysis. Given its rarity, the diagnosis can be challenging and may require ruling out other causes of eosinophilia (an elevated eosinophil count).
Key Diagnostic Approaches
- Blood Tests: A complete blood count (CBC) is typically the first step, revealing elevated eosinophil levels in the peripheral blood. In CEL, eosinophil counts often exceed 1,500 cells per microliter of blood.
- Bone Marrow Biopsy: A bone marrow biopsy is crucial for confirming the diagnosis. The bone marrow will show a significant increase in eosinophils, as well as potential abnormalities in cell morphology.
- Genetic Testing: Genetic mutations, particularly the FIP1L1-PDGFRα fusion gene, are frequently found in patients with CEL. Molecular analysis through polymerase chain reaction (PCR) can help identify these mutations and distinguish CEL from other forms of leukemia.
- Imaging Studies: Imaging techniques such as ultrasound or CT scans may be used to evaluate organ enlargement and assess the extent of tissue infiltration by eosinophils.
Treatment Options for Chronic Eosinophilic Leukemia
The treatment of chronic eosinophilic leukemia focuses on reducing eosinophil levels, alleviating symptoms, and preventing complications. Due to the rarity and complexity of CEL, management strategies are often tailored to the individual patient.
1. Targeted Therapy
Targeted therapies, particularly those targeting the abnormal PDGFRα (platelet-derived growth factor receptor alpha) fusion protein, have shown promising results in treating CEL. The use of tyrosine kinase inhibitors, such as imatinib (Gleevec), has significantly improved patient outcomes by specifically inhibiting the signaling pathways that drive eosinophil proliferation.
2. Chemotherapy
Chemotherapy may be used in more aggressive cases of CEL or when targeted therapies are ineffective. Chemotherapeutic agents, such as cytarabine and hydroxyurea, can help reduce the number of eosinophils in the blood and bone marrow. However, chemotherapy carries risks, including immune suppression and potential organ damage.
3. Corticosteroids
Corticosteroids, such as prednisone, are often prescribed to reduce inflammation and suppress the overactive immune response in CEL. They can help manage symptoms like skin rashes, joint pain, and gastrointestinal issues, but long-term use may lead to side effects such as osteoporosis and glucose intolerance.
4. Stem Cell Transplantation
In cases where CEL is resistant to other treatments or progresses to acute eosinophilic leukemia, stem cell transplantation (bone marrow transplant) may be considered. This procedure offers a potential cure by replacing the diseased bone marrow with healthy stem cells from a donor.
5. Supportive Care
Patients with CEL may also benefit from supportive treatments, such as blood transfusions to address anemia, pain management for organ involvement, and treatment of secondary infections due to immune system dysfunction.
Prognosis and Survival Rates
The prognosis for patients with chronic eosinophilic leukemia varies depending on several factors, including the presence of genetic mutations, the extent of organ involvement, and the response to treatment. The disease can often be managed effectively with targeted therapies, and many patients can achieve remission or a long period of stable disease. However, the risk of transformation to acute leukemia or organ failure remains a concern, especially in untreated or refractory cases.
Survival rates for CEL patients are generally favorable with appropriate treatment, with some studies indicating a 5-year survival rate of approximately 60-80%. Early diagnosis and prompt intervention are key to improving outcomes and quality of life for patients.