chronic diarrhea due to bile acid malabsorption can significantly impact an individual’s quality of life, with one common yet often overlooked cause being bile acid malabsorption (BAM). BAM is a gastrointestinal disorder where excess bile acids enter the colon, causing distressing symptoms such as chronic diarrhea. Understanding the mechanisms behind BAM, its diagnosis, and treatment options is crucial for both healthcare providers and patients.

What is Bile Acid Malabsorption (BAM)?
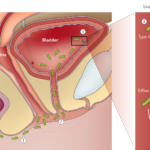
Bile acid malabsorption is a condition where the normal absorption of bile acids, which are produced in the liver and stored in the gallbladder, is disrupted. These bile acids are essential for the digestion and absorption of fats in the small intestine. When BAM occurs, bile acids are not properly reabsorbed in the ileum (the last part of the small intestine), leading them to accumulate in the colon, which can irritate the colon lining and cause chronic diarrhea.
Types of Bile Acid Malabsorption
There are two main types of BAM:
- Primary BAM: This occurs due to inherent defects in the bile acid transport mechanisms in the ileum, often seen in conditions like Crohn’s disease or ileal resections.
- Secondary BAM: This is more common and is caused by underlying gastrointestinal diseases that affect the normal bile acid reabsorption process, such as irritable bowel syndrome (IBS), celiac disease, or previous abdominal surgeries.
Causes of Chronic Diarrhea Due to BAM
Several factors can contribute to bile acid malabsorption and, consequently, chronic diarrhea:
- Ileal Disease or Resection: The most common cause of BAM is diseases that directly affect the ileum, such as Crohn’s disease or surgeries that remove part of the ileum.
- Post-surgical Changes: Patients who have undergone gallbladder removal or other abdominal surgeries may develop BAM as the body adjusts to altered bile acid metabolism.
- Small Intestinal Bacterial Overgrowth (SIBO): An overgrowth of bacteria in the small intestine can interfere with bile acid metabolism, leading to BAM.
- Genetic Factors: Certain genetic mutations can impair bile acid transporters in the ileum, resulting in primary BAM.
Symptoms of Chronic Diarrhea Due to BAM
The hallmark symptom of BAM is chronic diarrhea, but it can be accompanied by other gastrointestinal issues. Common symptoms include:
- Frequent, watery diarrhea: Often worse after eating, particularly meals high in fat.
- Urgency: A sudden, overwhelming need to use the bathroom.
- Abdominal pain: Cramping or bloating, which may intensify after meals.
- Weight loss: Due to malabsorption of fats and nutrients.
- Fatty stools (steatorrhea): Stools may appear pale, bulky, and greasy due to the poor digestion of fats.
- Flatulence: Excessive gas can occur as a result of impaired digestion.
Diagnosis of BAM
Diagnosing bile acid malabsorption requires a combination of clinical symptoms and specialized tests. Several methods can help identify BAM:
1. SeHCAT Test
The SeHCAT (Se-75 homocholic acid taurine) test is considered the gold standard for diagnosing BAM. It involves ingesting a radiolabeled bile acid and tracking its retention in the body. A low retention rate of bile acids indicates BAM.
2. Fecal Bile Acid Testing
This test measures the concentration of bile acids in the stool. High levels of bile acids in the stool suggest that bile acids are not being absorbed properly in the small intestine.
3. Imaging and Endoscopy
In some cases, doctors may recommend imaging tests or endoscopy to check for underlying conditions, such as Crohn’s disease or intestinal surgeries, which can contribute to BAM.
4. Bile Acid Malabsorption Questionnaire (BAM-Q)
A clinical tool used by healthcare providers to assess the likelihood of BAM in patients presenting with chronic diarrhea.
Treatment and Management of Chronic Diarrhea Due to BAM
Managing chronic diarrhea due to bile acid malabsorption typically involves dietary adjustments, medications, and in some cases, surgical interventions. The treatment strategy varies depending on the underlying cause of BAM.
1. Medications for BAM
- Bile Acid Sequestrants: Medications like cholestyramine, colesevelam, and colestipol are commonly used to bind excess bile acids in the intestines and reduce diarrhea. These drugs help prevent bile acids from reaching the colon, thereby alleviating symptoms.
- Antidiarrheal Agents: Drugs like loperamide can provide symptom relief by slowing down bowel movements and reducing diarrhea episodes.
2. Dietary Modifications
Patients with BAM should follow a low-fat diet to minimize the impact of bile acids on the colon. The use of medium-chain triglycerides (MCT) oils, which do not require bile acids for digestion, can be beneficial. Additionally, reducing the intake of fatty, greasy foods can help manage symptoms.
3. Probiotics and Prebiotics
In some cases, probiotics may help restore the balance of gut bacteria, which can improve digestion and reduce diarrhea. Prebiotics can also be used to support gut health and enhance the function of beneficial bacteria.
4. Surgical Interventions
In rare cases where BAM is severe and resistant to treatment, surgical options may be considered, such as ileal bypass or surgical removal of affected sections of the intestine.
Lifestyle and Coping Strategies for Patients with BAM
Living with chronic diarrhea due to bile acid malabsorption can be challenging, but several strategies can help patients manage their condition effectively:
- Maintaining Hydration: Chronic diarrhea can lead to dehydration, so it’s essential to drink plenty of fluids throughout the day. Oral rehydration solutions may be helpful for restoring lost electrolytes.
- Stress Management: Stress can exacerbate gastrointestinal symptoms, so techniques like yoga, meditation, or mindfulness may provide relief.
- Frequent Small Meals: Eating smaller meals more frequently can reduce the burden on the digestive system and help manage symptoms better than large meals.