Chromoblastomycosis is a chronic fungal infection that predominantly affects the skin and subcutaneous tissues. Caused by various species of dematiaceous fungi, this infection leads to the formation of distinct lesions and, if left untreated, can cause significant health complications. While it is more common in tropical and subtropical regions, its global incidence continues to be a concern. In this comprehensive article, we will explore the key aspects of chromoblastomycosis, from its symptoms and diagnostic approaches to available treatment strategies and prevention methods.
What is Chromoblastomycosis?
Chromoblastomycosis is a skin infection primarily caused by darkly pigmented (dematiaceous) fungi. These fungi, including species such as Fonsecaea, Cladophialophora, and Phialophora, invade the skin when the spores come into contact with broken skin, typically through trauma like cuts or abrasions. The condition is characterized by the appearance of raised, scaly, and wart-like lesions on the skin. It progresses slowly, leading to more extensive tissue damage if left untreated.
The Fungal Pathogen
The organisms responsible for chromoblastomycosis are generally soil-dwelling fungi. They thrive in humid, tropical, and subtropical environments. The spores of these fungi enter the body through minor injuries and cause infection in susceptible individuals. People who work outdoors or engage in activities like farming, construction, and forestry are at a higher risk of contracting the infection.
Symptoms of Chromoblastomycosis
The symptoms of chromoblastomycosis can vary depending on the severity of the infection. Initially, the infection manifests as a small, painless bump or nodule on the skin. Over time, these bumps may grow, becoming larger and more noticeable, often resembling warts or cauliflower-like structures.
Early-Stage Symptoms
- Small, raised, pigmented nodules
- Itchy or mildly painful skin lesions
- Occasional swelling at the infection site
Progressive Symptoms
As the infection spreads, more symptoms may develop:
- Thickening and crusting of skin lesions
- Ulceration at the site of infection
- Formation of multiple lesions
- Possible tissue necrosis in severe cases
If untreated, chromoblastomycosis can spread to deeper tissues, such as the bones, and result in more significant health issues.
Diagnosing Chromoblastomycosis
A comprehensive diagnostic approach is crucial in identifying chromoblastomycosis. The condition can often be mistaken for other skin infections or disorders, so it is essential for healthcare professionals to conduct a detailed assessment.
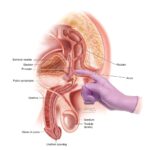
Clinical Examination
Healthcare providers will start by examining the characteristic appearance of the lesions. These lesions are often raised, discolored, and show signs of chronic inflammation. The doctor will look for the characteristic “cobblestone” appearance of the lesions, which is common in chromoblastomycosis.
Laboratory Tests
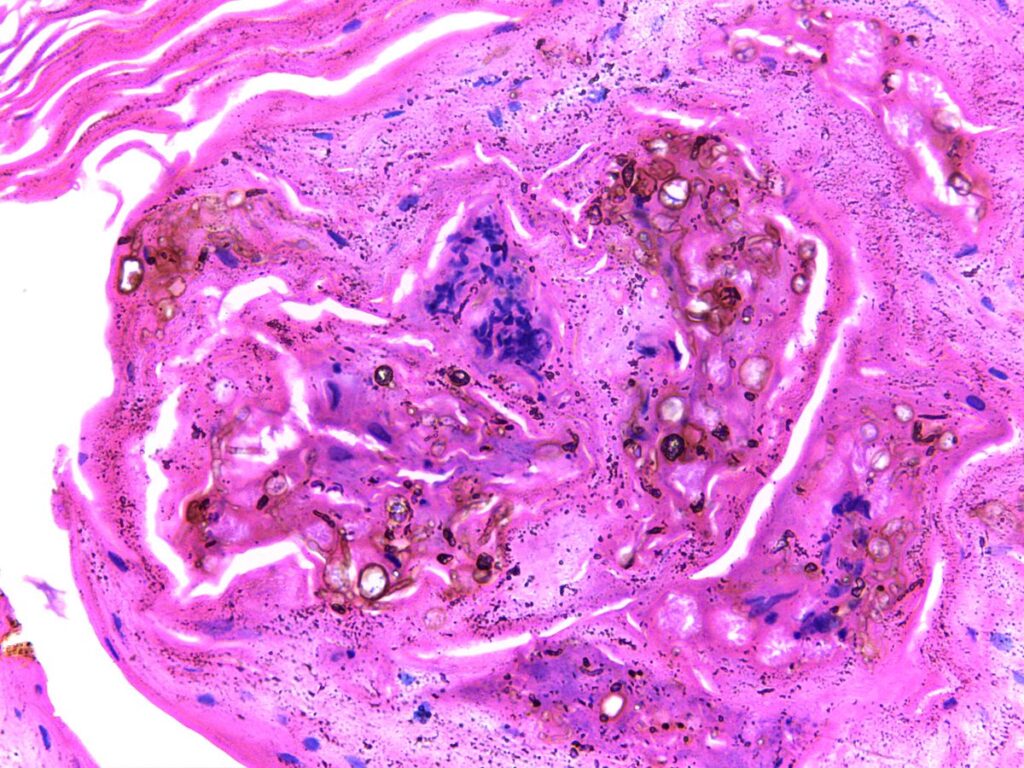
- Microscopic Examination: Skin scrapings from the lesions are examined under a microscope. The presence of fungal elements, such as the characteristic round or oval fungal cells, helps confirm the diagnosis.
- Culture: Fungal cultures are essential for identifying the specific causative organism. Cultures can help differentiate chromoblastomycosis from other skin conditions caused by different pathogens.
- Histopathology: A biopsy of the affected tissue is often performed to analyze the fungal invasion and tissue response in more detail.
Imaging Studies
In severe cases, when the infection spreads to deeper tissues, imaging studies may be required to assess the extent of tissue involvement.
Treatment Options for Chromoblastomycosis
Treating chromoblastomycosis can be challenging, especially in chronic cases. The choice of treatment depends on the severity of the infection, the species of fungi involved, and the patient’s overall health.
Antifungal Medications
The primary treatment for chromoblastomycosis involves the use of antifungal agents. Commonly prescribed antifungals include:
- Itraconazole: This is the first-line treatment for chromoblastomycosis and is often effective in treating localized cases.
- Terbinafine: This medication may be prescribed in some cases, especially if itraconazole is not effective.
- Fluconazole and Ketoconazole: These may be used when other treatments fail or for cases involving specific fungal species.
The duration of antifungal therapy can range from several months to over a year, depending on the extent of the infection and the patient’s response to treatment.
Surgical Interventions
In some cases, especially when there are large, deeply infiltrating lesions, surgical removal of the affected tissue may be necessary. Surgery is often combined with antifungal treatment to improve outcomes.
Cryotherapy and Laser Therapy
In select cases, cryotherapy (freezing) and laser therapy can be used to treat localized skin lesions. These methods are typically considered for cosmetic reasons or when the lesions do not respond to conventional treatments.
Adjunctive Therapies
Patients may also benefit from adjunctive therapies, such as corticosteroids to manage inflammation or other medications to address secondary infections.
Preventing Chromoblastomycosis
Prevention of chromoblastomycosis is primarily centered around minimizing the risk of fungal exposure. Although there are no specific vaccines or prophylactic treatments available, certain precautions can significantly reduce the risk of infection.
Protective Measures
- Wearing Protective Clothing: Individuals working in environments with soil exposure should wear long sleeves, gloves, and other protective clothing to prevent cuts and abrasions.
- Proper Wound Care: Promptly cleaning and dressing any cuts, abrasions, or puncture wounds reduces the risk of fungal infection.
- Avoiding High-Risk Areas: People should be cautious when handling decaying plant matter or soil in areas known to harbor these fungi.
Early Detection and Treatment
Early diagnosis and prompt treatment are critical in preventing the progression of chromoblastomycosis. Individuals who notice unusual skin lesions, especially if they are persistent and resistant to standard treatments, should seek medical attention immediately.
The Prognosis of Chromoblastomycosis
With early diagnosis and appropriate treatment, the prognosis for chromoblastomycosis is generally positive. However, in severe or untreated cases, the infection can lead to complications such as deep tissue involvement, scarring, and functional impairment. Long-term antifungal therapy may be required for individuals with chronic or extensive disease.
Chromoblastomycosis remains a significant concern, particularly in tropical and subtropical regions. Its slow, progressive nature means that early recognition and intervention are essential for favorable outcomes. With advancements in diagnostic techniques and treatment options, individuals affected by this fungal infection can lead a normal life if managed appropriately. Public awareness and protective measures are also crucial in preventing new cases and minimizing the impact of this condition.