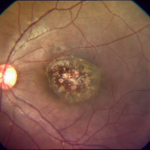
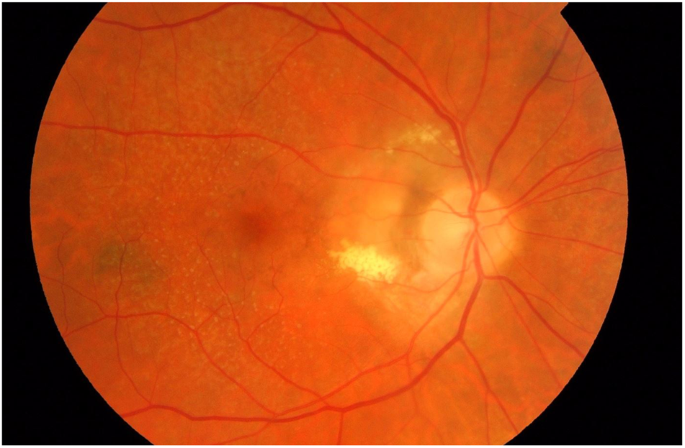
Choroidal neovascularization (CNV) is a pathological process characterized by the growth of new blood vessels originating from the choroid through Bruch’s membrane into the retinal pigment epithelium (RPE) and retina. This condition is commonly associated with various retinal diseases and is a leading cause of vision loss globally. Understanding its causes, clinical manifestations, diagnostic techniques, and treatment modalities is crucial for effective management.
Understanding Choroidal Neovascularization
CNV occurs when the normal balance of angiogenic and anti-angiogenic factors is disrupted, leading to abnormal vascular proliferation. These newly formed blood vessels are often fragile and prone to leakage, causing fluid accumulation, hemorrhage, and scarring that can significantly impair vision.
Common Causes and Associated Conditions
- Age-Related Macular Degeneration (AMD): CNV is a hallmark of neovascular (wet) AMD, a leading cause of blindness in older adults.
- Pathologic Myopia: High myopia can lead to mechanical stretching and degeneration of retinal structures, predisposing to CNV.
- Central Serous Chorioretinopathy (CSCR): Chronic CSCR can result in RPE damage, increasing the risk of CNV.
- Ocular Trauma or Inflammation: Conditions like posterior uveitis and choroiditis may trigger CNV.
- Inherited Retinal Diseases: Rare genetic disorders, such as Best disease or Stargardt’s disease, may be complicated by CNV.
Clinical Presentation
The symptoms of CNV can vary depending on the extent and location of the lesion but often include:
- Sudden or gradual central vision loss.
- Distorted vision (metamorphopsia).
- Dark or blurry spots in the central visual field (scotomas).
- Reduced contrast sensitivity.
Diagnostic Approaches
Accurate and early diagnosis of CNV is essential for preserving vision. The following diagnostic tools are commonly employed:
1. Optical Coherence Tomography (OCT):
OCT provides high-resolution cross-sectional imaging of retinal layers, revealing fluid accumulation, retinal thickening, or pigment epithelial detachment.
2. Fluorescein Angiography (FA):
This technique uses fluorescein dye to identify leakage from abnormal blood vessels, confirming the presence and activity of CNV.
3. Indocyanine Green Angiography (ICGA):
ICGA is particularly useful for visualizing the choroidal vasculature and diagnosing polypoidal choroidal vasculopathy, a subtype of CNV.
4. Fundus Examination:
Dilated fundus examination helps in identifying subretinal hemorrhage, exudates, and other retinal changes associated with CNV.
Treatment Options
Advancements in treatment have significantly improved the prognosis for CNV. The primary treatment strategies include:
1. Anti-Vascular Endothelial Growth Factor (Anti-VEGF) Therapy:
Anti-VEGF drugs, such as ranibizumab, aflibercept, and bevacizumab, are the first-line treatment for CNV. These medications inhibit VEGF, a key mediator of angiogenesis, reducing leakage and preventing further vessel growth. Regular intravitreal injections are often required.
2. Photodynamic Therapy (PDT):
PDT involves intravenous administration of a photosensitizing agent followed by activation with a specific wavelength of laser light. This therapy selectively targets abnormal blood vessels while sparing surrounding healthy tissue.
3. Thermal Laser Photocoagulation:
Though less commonly used, laser photocoagulation may be effective for well-defined extrafoveal CNV lesions. However, it carries a risk of collateral damage to adjacent retinal tissue.
4. Combination Therapy:
Combining anti-VEGF therapy with PDT or corticosteroids may be beneficial in certain refractory cases.
5. Surgical Options:
In rare cases, surgical intervention such as macular translocation or subretinal surgery may be considered for CNV associated with extensive scarring or hemorrhage.
Prognosis and Follow-Up
The visual outcome in CNV depends on early diagnosis and timely intervention. Regular monitoring using OCT and other imaging modalities is essential to detect disease progression and guide treatment adjustments. Patient education regarding symptom recognition and adherence to follow-up schedules is equally vital.
Prevention and Risk Mitigation
While not all cases of CNV are preventable, certain strategies can reduce risk:
- Regular eye examinations, especially for individuals at high risk (e.g., AMD or myopia patients).
- Smoking cessation to lower the risk of AMD-related CNV.
- Maintaining a healthy lifestyle with a balanced diet rich in antioxidants and omega-3 fatty acids.