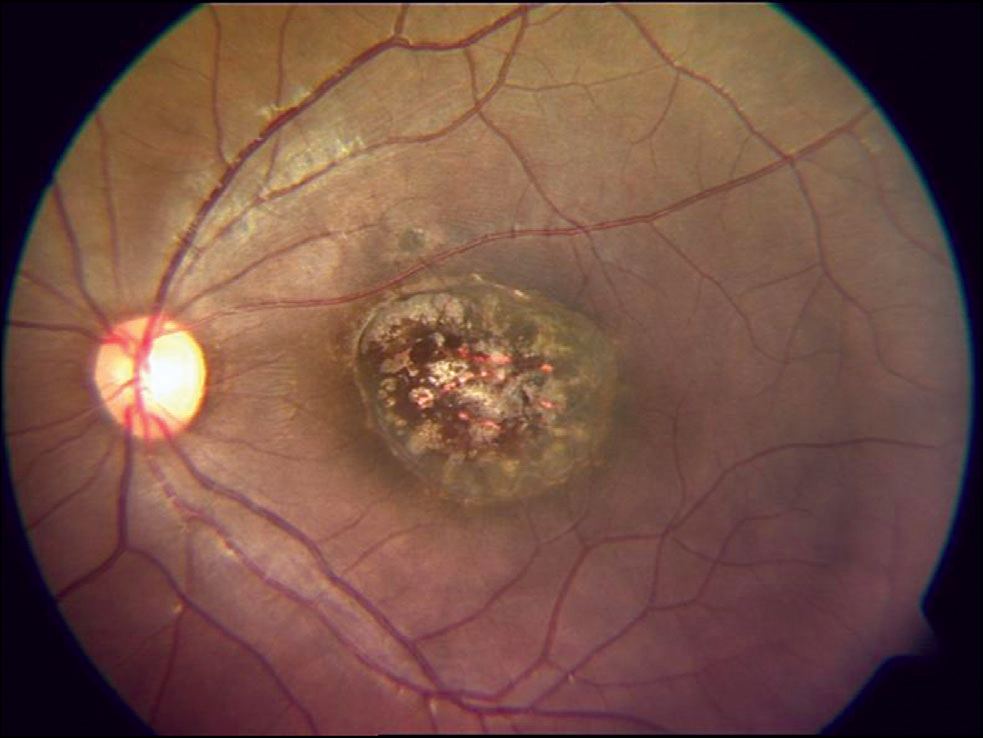
Chorioretinitis, a serious eye condition, involves inflammation of the choroid and retina, two vital layers of the eye that are essential for clear vision. Early recognition and appropriate management are critical to preserving vision and preventing complications.
What is Chorioretinitis?
Chorioretinitis is a form of posterior uveitis that primarily affects the choroid (a vascular layer supplying nutrients to the retina) and the retina (the light-sensitive tissue at the back of the eye). The condition can lead to scarring, vision impairment, and, in severe cases, irreversible blindness if left untreated.
Causes of Chorioretinitis
The inflammation in chorioretinitis can arise due to various infectious and non-infectious causes. Below are the primary triggers
1. Infectious Causes
- Toxoplasmosis: The most common cause of infectious chorioretinitis, often linked to the parasite Toxoplasma gondii. Congenital and acquired infections are possible.
- Cytomegalovirus (CMV): Commonly seen in immunocompromised individuals, such as those with HIV/AIDS.
- Syphilis: A sexually transmitted infection caused by Treponema pallidum.
- Tuberculosis (TB): Ocular manifestations of systemic TB can include chorioretinitis.
- Herpes Simplex Virus (HSV) and Varicella-Zoster Virus (VZV): Can cause necrotizing retinitis leading to chorioretinitis.
- Fungal Infections: Opportunistic fungi like Candida albicans can cause endophthalmitis with chorioretinitis.
2. Non-Infectious Causes
- Autoimmune Disorders: Conditions like Behçet’s disease or sarcoidosis may provoke inflammation in the eye.
- Idiopathic: In some cases, no specific cause can be identified.
Symptoms of Chorioretinitis
The symptoms of chorioretinitis often develop gradually but can vary depending on the underlying cause and severity. Common signs include:
- Blurred Vision: A hallmark symptom caused by retinal involvement.
- Floaters: Spots or shadows in the visual field.
- Photophobia: Sensitivity to light.
- Eye Pain: Can occur in cases with severe inflammation.
- Redness: Though less common, redness may accompany systemic infections.
- Reduced Peripheral Vision: In advanced or untreated cases.
Early detection is key to managing the condition and preventing complications such as retinal detachment or permanent vision loss.
Diagnosis of Chorioretinitis
Diagnosing chorioretinitis involves a thorough clinical evaluation and diagnostic tests to identify the underlying cause. The following methods are commonly used:
1. Clinical Examination
- Fundoscopy: To observe lesions or inflammation in the retina and choroid.
- Slit-Lamp Biomicroscopy: For anterior segment evaluation and vitreous involvement.
2. Imaging Studies
- Optical Coherence Tomography (OCT): Provides detailed cross-sectional images of retinal layers.
- Fluorescein Angiography (FA): Helps visualize retinal blood flow and detect leakage or lesions.
- Indocyanine Green Angiography (ICG): Used to evaluate choroidal blood vessels.
3. Laboratory Tests
- Serological Testing: Detects specific infectious agents like Toxoplasma or Treponema pallidum.
- Polymerase Chain Reaction (PCR): Identifies pathogens in aqueous or vitreous humor.
- General Blood Tests: Includes complete blood count (CBC), inflammatory markers (ESR, CRP), and tests for autoimmune disorders.
Treatment Options for Chorioretinitis
Effective treatment of chorioretinitis targets the underlying cause and manages inflammation. Depending on the etiology, the following therapeutic approaches are utilized:
1. Pharmacological Treatment
- Corticosteroids: Administered as oral, topical, or intravitreal injections to reduce inflammation.
- Antimicrobial Therapy:
- Antibiotics: For bacterial infections like syphilis or tuberculosis.
- Antiviral Drugs: Such as ganciclovir or valganciclovir for viral causes.
- Antifungal Agents: For fungal infections like candidiasis.
- Immunosuppressive Agents: Used in autoimmune-related chorioretinitis.
2. Surgical Interventions
- Vitrectomy: May be required in severe cases to remove vitreous opacities or repair retinal detachment.
- Laser Photocoagulation: To prevent further damage in conditions like retinal neovascularization.
3. Supportive Measures
- Regular follow-ups to monitor progression.
- Management of systemic diseases to prevent recurrence.
Prognosis and Prevention
The prognosis of chorioretinitis largely depends on the timeliness and adequacy of treatment. With prompt intervention, most cases can be managed effectively, preserving vision.
Prevention Tips:
- Hygiene Practices: To prevent infections like toxoplasmosis.
- Routine Eye Exams: Especially for individuals with autoimmune disorders or systemic infections.
- Prompt Medical Attention: Seek immediate care for symptoms like blurred vision or floaters.