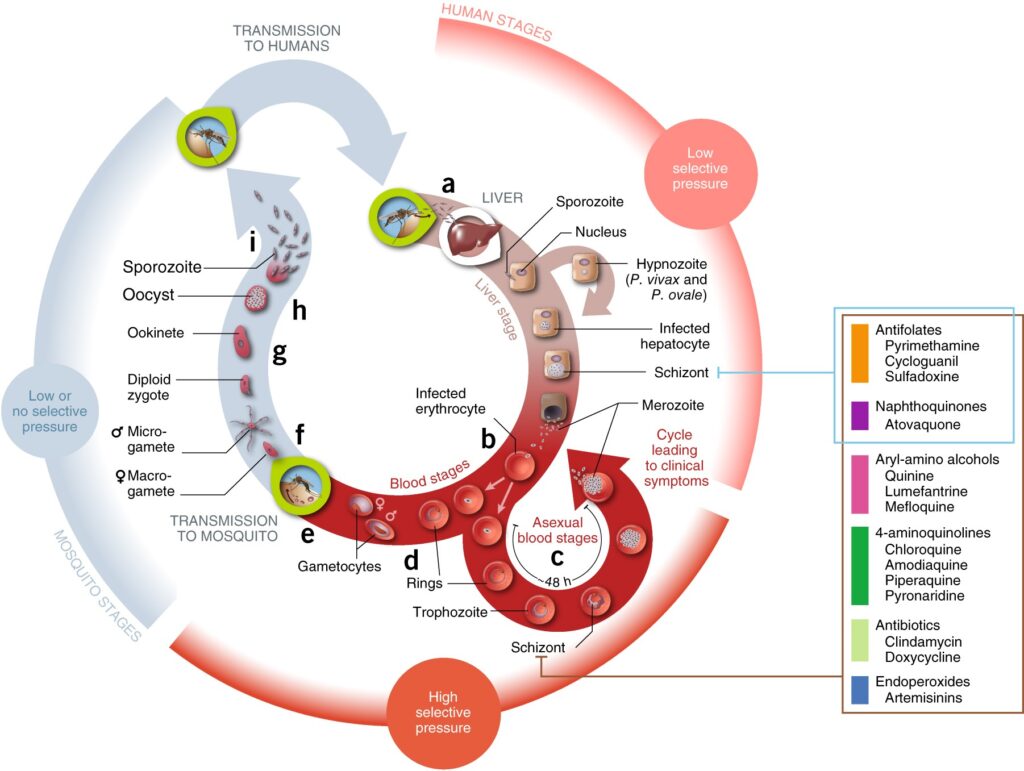
Malaria, caused by the Plasmodium parasite, continues to pose a significant public health challenge globally. Among the five Plasmodium species that infect humans, Plasmodium falciparum is the most lethal, accounting for the majority of malaria-related deaths. The emergence and spread of chloroquine-resistant Plasmodium falciparum strains have severely undermined malaria control efforts and necessitate urgent action. This article provides an in-depth exploration of chloroquine resistance, its mechanisms, epidemiology, and effective management strategies.
Mechanisms of Chloroquine Resistance
Chloroquine, once a frontline antimalarial drug, functions by disrupting the detoxification of heme in the parasite’s food vacuole. Resistance to chloroquine is primarily attributed to mutations in the Plasmodium falciparum chloroquine resistance transporter (PfCRT) gene. These mutations alter the drug’s accumulation within the food vacuole, rendering it ineffective against the parasite.
Key Genetic Mutations
- PfCRT Mutations: The K76T mutation in the PfCRT gene is a hallmark of chloroquine resistance, accompanied by other polymorphisms that enhance resistance levels.
- Additional Modifiers: Mutations in other genes, such as PfMDR1 (multidrug resistance gene 1), further influence resistance phenotypes.
Evolutionary Factors
- Drug Pressure: Prolonged and widespread use of chloroquine exerted selective pressure, enabling resistant strains to proliferate.
- Genetic Bottlenecks: The transmission of resistant alleles through population bottlenecks facilitated their establishment in endemic regions.
Epidemiology of Chloroquine-Resistant Malaria
Chloroquine resistance was first identified in Southeast Asia and South America in the late 1950s. It subsequently spread to sub-Saharan Africa, where malaria burden is highest. Today, chloroquine resistance is nearly ubiquitous in Plasmodium falciparum endemic areas.
Global Distribution
- Africa: Resistance is widespread, contributing to the shift towards artemisinin-based combination therapies (ACTs).
- Asia and South America: Resistance remains prevalent, with additional resistance to other antimalarial drugs compounding the challenge.
Impact on Malaria Control
- Increased Mortality: The decline in chloroquine efficacy has resulted in higher morbidity and mortality rates, particularly in regions with limited access to alternative therapies.
- Economic Burden: Resistant malaria strains necessitate more expensive treatments, straining healthcare systems in low-resource settings.
Clinical Implications and Treatment Options
Current Treatment Guidelines
The World Health Organization (WHO) recommends ACTs as the first-line treatment for Plasmodium falciparum malaria. These therapies combine artemisinin derivatives with partner drugs to delay resistance development.
Challenges in Treatment
- Drug Resistance: Emerging resistance to artemisinin and partner drugs poses a significant threat to current treatment protocols.
- Access to Medication: Limited availability of ACTs in remote areas exacerbates the burden of chloroquine-resistant malaria.
Future Therapeutic Strategies
- Novel Drug Development: Research focuses on developing new antimalarial compounds targeting alternative pathways in the parasite.
- Combination Therapies: Combining existing drugs with synergistic mechanisms aims to enhance efficacy and prevent resistance.
Prevention and Control Measures
Vector Control
- Insecticide-Treated Nets (ITNs): Effective in reducing malaria transmission by protecting individuals from mosquito bites.
- Indoor Residual Spraying (IRS): Targets mosquito vectors within households, curbing their populations.
Surveillance and Monitoring
- Resistance Tracking: Regular monitoring of drug efficacy and resistance patterns is crucial for adapting treatment policies.
- Genetic Studies: Analyzing parasite genomes helps identify emerging resistance mutations and informs drug development.
Public Health Interventions
- Community Awareness: Educating populations on the proper use of antimalarial drugs and preventive measures.
- Integrated Strategies: Combining vector control, chemotherapy, and surveillance to achieve sustained malaria reduction.
MYHEALTHMAG

