Abnormal uterine bleeding (AUB) is a common condition affecting women of reproductive age, as well as those who are perimenopausal or postmenopausal. It is characterized by bleeding from the uterus that is irregular in frequency, duration, or amount. This condition can be distressing and may indicate underlying health issues. Early diagnosis and appropriate treatment are crucial to managing symptoms and preventing potential complications.

What is Abnormal Uterine Bleeding?
Abnormal uterine bleeding refers to any deviation from a normal menstrual cycle. Normal menstruation typically occurs every 21 to 35 days and lasts between 2 to 7 days. Any bleeding outside these parameters, whether it is too heavy, too frequent, or too prolonged, is considered abnormal. AUB can occur as a result of hormonal imbalances, structural abnormalities, or underlying medical conditions, and it is important to seek medical evaluation if the bleeding is persistent or causes significant distress.
Causes of Abnormal Uterine Bleeding
A variety of factors can contribute to abnormal uterine bleeding. These causes can be categorized into several broad categories, including hormonal imbalances, structural issues, and medical conditions.
Hormonal Imbalances
Hormonal fluctuations are one of the most common causes of abnormal uterine bleeding, particularly in women during their reproductive years. Hormonal imbalances often occur during puberty, perimenopause, or with the use of hormonal contraceptives.
- Anovulation: This occurs when the ovaries do not release an egg during the menstrual cycle. It is common in women with polycystic ovary syndrome (PCOS), thyroid disorders, or those who are undergoing significant weight changes.
- Estrogen Dominance: When the body produces too much estrogen without enough progesterone to counterbalance it, this can lead to endometrial thickening and heavy bleeding.
- Menopause: As women approach menopause, they experience fluctuating hormone levels, which can cause irregular bleeding patterns.
Structural Abnormalities
Structural issues within the reproductive system can also cause abnormal bleeding. These include:
- Uterine Fibroids: These noncancerous tumors, often made of muscle tissue, can cause heavy or prolonged menstrual bleeding. They are particularly common in women of reproductive age.
- Polyps: Endometrial polyps are growths on the inner lining of the uterus that can cause irregular bleeding.
- Adenomyosis: This condition occurs when the endometrial tissue grows into the muscle wall of the uterus, leading to heavy menstrual bleeding and pelvic pain.
- Endometrial Hyperplasia: An overgrowth of the uterine lining, often caused by an imbalance of estrogen and progesterone, which can result in heavy bleeding.
- Cancer: In rare cases, uterine or endometrial cancer can cause abnormal bleeding, particularly in postmenopausal women.
Medical Conditions
Several underlying medical conditions can also lead to abnormal uterine bleeding. These include:
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can cause menstrual irregularities, including heavy or irregular bleeding.
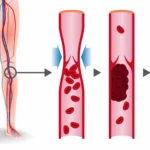
- Coagulation Disorders: Conditions such as von Willebrand disease or platelet dysfunction can lead to abnormal bleeding, including heavy menstrual flow.
- Diabetes and Obesity: These conditions can affect hormonal balance, leading to abnormal uterine bleeding.
- Medications: Certain medications, including anticoagulants, can increase the risk of abnormal bleeding.
Symptoms of Abnormal Uterine Bleeding
The symptoms of abnormal uterine bleeding can vary, but common signs include:
- Heavy menstrual bleeding (menorrhagia): Soaking through one or more sanitary pads or tampons every hour for several consecutive hours.
- Prolonged bleeding: Menstrual bleeding lasting longer than 7 days.
- Irregular bleeding: Bleeding between periods or after menopause.
- Spotting: Light bleeding or spotting that occurs outside of regular menstrual cycles.
- Painful periods (dysmenorrhea): Severe cramping or pelvic pain associated with menstruation.
If these symptoms are persistent or severe, it is essential to consult a healthcare provider to determine the cause and appropriate treatment.
Diagnosing Abnormal Uterine Bleeding
A thorough evaluation is necessary to diagnose the cause of abnormal uterine bleeding. The diagnostic process typically involves the following:
Medical History and Physical Examination
The healthcare provider will begin by taking a detailed medical history, including menstrual history, any prior gynecological issues, and lifestyle factors. A physical examination may include a pelvic exam to check for signs of fibroids, cysts, or other abnormalities.
Laboratory Tests
- Blood Tests: Blood tests may be ordered to check for anemia (due to heavy bleeding) or hormonal imbalances, including thyroid function tests and coagulation profiles.
- Endometrial Biopsy: A small sample of the uterine lining may be taken to check for abnormal cells, including cancer.
- Pap Smear: A routine Pap smear can help screen for cervical cancer, which can sometimes cause abnormal bleeding.
Imaging Tests
- Ultrasound: A pelvic ultrasound is a non-invasive test that can detect uterine fibroids, polyps, and other structural abnormalities.
- Hysteroscopy: In this procedure, a small camera is inserted into the uterus to directly visualize the uterine lining and any abnormalities.
- Sonohysterography: This is a type of ultrasound where a saline solution is injected into the uterus to get a better view of the uterine lining.
Treatment Options for Abnormal Uterine Bleeding
The treatment for abnormal uterine bleeding depends on the underlying cause, the severity of the symptoms, and the patient’s reproductive goals. The following options may be considered:
1. Hormonal Therapy
- Birth Control Pills: Oral contraceptives can help regulate the menstrual cycle and reduce heavy bleeding by controlling hormonal fluctuations.
- Progestin Therapy: Progestin can be used to counteract the effects of estrogen and reduce endometrial lining growth, helping to control bleeding.
- Intrauterine Device (IUD): A hormonal IUD can reduce bleeding and provide long-term contraception.
- GnRH Agonists: These drugs temporarily induce a menopause-like state to shrink fibroids and control heavy bleeding.
2. Surgical Interventions
- Dilation and Curettage (D&C): This procedure involves scraping the uterine lining to remove any abnormal tissue and alleviate heavy bleeding.
- Endometrial Ablation: This minimally invasive procedure destroys the uterine lining to stop bleeding.
- Myomectomy: If fibroids are the cause of bleeding, a myomectomy may be performed to remove the fibroids while preserving the uterus.
- Hysterectomy: In severe cases where other treatments are ineffective, a hysterectomy (removal of the uterus) may be recommended, especially in women who are past childbearing age.
3. Non-Surgical Treatments
- Tranexamic Acid: This medication helps reduce bleeding by promoting blood clotting.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen, can help control pain and reduce heavy bleeding.
- Iron Supplements: If heavy bleeding has led to anemia, iron supplements may be prescribed to restore healthy iron levels.
Prevention of Abnormal Uterine Bleeding
While it may not always be possible to prevent abnormal uterine bleeding, several lifestyle factors can reduce the risk:
- Regular Gynecological Check-ups: Routine visits to a healthcare provider for screenings and early detection of abnormalities can help prevent complications.
- Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and a healthy weight can help regulate hormonal balance and reduce the risk of conditions like fibroids and endometrial cancer.
- Managing Stress: High levels of stress can disrupt hormonal balance, contributing to irregular bleeding. Stress management techniques, such as yoga and mindfulness, can help.
Abnormal uterine bleeding is a complex condition with multiple potential causes, including hormonal imbalances, structural abnormalities, and underlying medical conditions. Early detection, thorough diagnosis, and appropriate treatment are essential to managing symptoms and preventing complications. With a range of treatment options available, from hormonal therapy to surgical interventions, women suffering from abnormal uterine bleeding can find relief and improve their quality of life. Regular check-ups and a healthy lifestyle can help reduce the risk of recurrence and promote overall reproductive health.