Chlamydia trachomatis is a significant bacterial pathogen responsible for various infections, most notably pelvic inflammatory disease (PID) in women. As one of the leading causes of reproductive health complications, understanding the relationship between Chlamydia trachomatis and PID is critical for prevention, early diagnosis, and effective treatment.
What is Chlamydia Trachomatis?
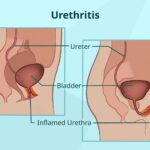
Chlamydia trachomatis is a gram-negative, obligate intracellular bacterium. It is the most prevalent sexually transmitted infection (STI) globally, affecting millions of individuals annually. The bacterium is classified into multiple serovars, with serovars D-K being primarily associated with urogenital infections.
Modes of Transmission
- Sexual Contact: Chlamydia trachomatis spreads through vaginal, anal, or oral sex with an infected partner.
- Vertical Transmission: Infected mothers can pass the bacterium to newborns during childbirth, leading to neonatal conjunctivitis or pneumonia.
Understanding Pelvic Inflammatory Disease (PID)
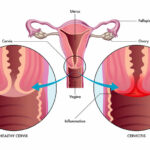
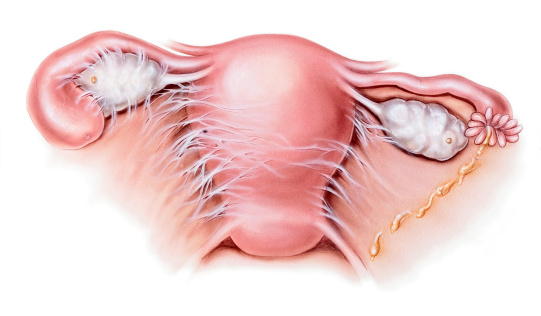
Pelvic inflammatory disease is a polymicrobial infection affecting the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It is often a complication of untreated sexually transmitted infections, with Chlamydia trachomatis being a primary causative agent.
Risk Factors
- Unprotected Sexual Activity: Increases exposure to STIs.
- Multiple Sexual Partners: Elevates the risk of infection.
- Previous PID Episodes: Predisposes to recurrent infections.
- Use of Intrauterine Devices (IUDs): During the initial weeks of insertion.
Symptoms of Chlamydia-Associated PID
The clinical presentation of PID varies, ranging from asymptomatic to severe symptoms. Common signs include:
- Lower Abdominal Pain: Often bilateral and persistent.
- Abnormal Vaginal Discharge: Typically purulent and foul-smelling.
- Dyspareunia: Pain during sexual intercourse.
- Irregular Menstrual Bleeding: Including intermenstrual spotting or post-coital bleeding.
- Fever and Malaise: Indicating systemic infection.
Pathophysiology of Chlamydia-Induced PID
Chlamydia trachomatis ascends from the lower genital tract to the upper reproductive organs, initiating an inflammatory response. The immune system’s attempt to combat the infection often results in tissue damage, scarring, and adhesions.
Diagnostic Approach
Accurate diagnosis is essential for effective management. Common diagnostic methods include:
- Nucleic Acid Amplification Tests (NAATs): Gold standard for detecting Chlamydia trachomatis in urogenital samples.
- Pelvic Examination: Identifies cervical motion tenderness, adnexal tenderness, and uterine tenderness.
- Ultrasound Imaging: Detects abscesses, fluid collections, or tubal thickening.
- Laparoscopy: A definitive method to visualize pelvic structures and confirm PID.
Treatment Options
Timely treatment can prevent long-term complications. The following therapeutic strategies are commonly employed:
Antibiotic Therapy
- Empirical Regimens: Combination therapy targeting Chlamydia trachomatis, Neisseria gonorrhoeae, and anaerobes.
- Doxycycline (100 mg twice daily for 14 days)
- Ceftriaxone (250 mg intramuscularly, single dose)
- Metronidazole (500 mg twice daily for 14 days)
Pain Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate discomfort.
Hospitalization
- Severe cases with abscess formation or systemic symptoms may require intravenous antibiotics and close monitoring.
Preventive Measures
Preventing Chlamydia trachomatis infections is key to reducing PID incidence. Effective measures include:
- Safe Sexual Practices: Consistent use of condoms and mutual monogamy.
- Regular Screening: Annual testing for sexually active individuals under 25 or those with risk factors.
- Timely Treatment: Immediate management of STIs to prevent complications.
- Partner Notification: Informing sexual partners to ensure treatment and break the chain of transmission.
Long-Term Complications
Untreated or inadequately managed Chlamydia-induced PID can lead to:
- Infertility: Due to tubal occlusion.
- Ectopic Pregnancy: Resulting from impaired tubal motility.
- Chronic Pelvic Pain: Caused by persistent inflammation or adhesions.
- Perihepatitis (Fitz-Hugh-Curtis Syndrome): Inflammation of the liver capsule.