Chemotherapy is a cornerstone in cancer treatment, but its effectiveness comes with a range of potential side effects. One of the most concerning and common complications is chemotherapy-induced neutropenia (CIN). This condition occurs when chemotherapy drugs lead to a significant decrease in the number of neutrophils, a type of white blood cell that plays a crucial role in fighting infections. Understanding the causes, symptoms, diagnosis, and treatment strategies for CIN is vital for optimizing patient care and reducing risks.
What Is Chemotherapy-Induced Neutropenia?
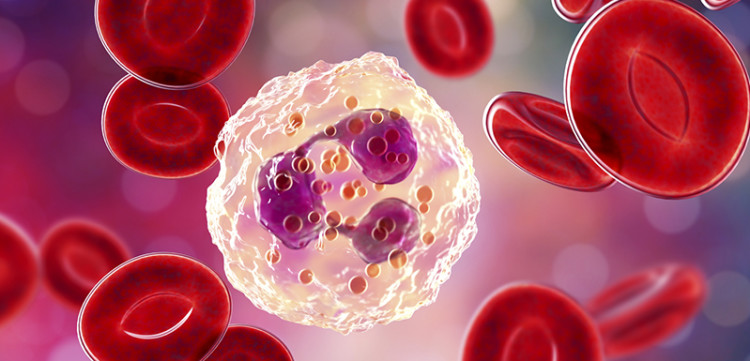
Chemotherapy-induced neutropenia (CIN) is a condition characterized by a drop in neutrophil levels due to the cytotoxic effects of chemotherapy drugs. Neutrophils are essential components of the immune system that help protect the body against bacterial infections. When neutrophil counts fall below the normal threshold, patients become highly vulnerable to infections, particularly those caused by bacteria, fungi, and viruses.
Causes of Chemotherapy-Induced Neutropenia
CIN is primarily caused by the impact of chemotherapy drugs on the bone marrow, where neutrophils are produced. Chemotherapy agents, particularly those used in high doses, can suppress bone marrow function, leading to reduced production of white blood cells. The following are common causes of CIN:
- Chemotherapy Drugs: Drugs such as cyclophosphamide, doxorubicin, paclitaxel, and carboplatin are known to be particularly myelosuppressive, meaning they interfere with the bone marrow’s ability to produce cells.
- Bone Marrow Sensitivity: Some patients’ bone marrow may be more sensitive to chemotherapy, increasing the risk of CIN.
- Chemotherapy Dosage and Schedule: Higher doses or more frequent administration schedules of chemotherapy drugs may result in more severe neutropenia.
- Combination Therapies: When chemotherapy is combined with other treatments, such as targeted therapies or immunotherapy, the risk of CIN can increase.
Symptoms of Chemotherapy-Induced Neutropenia
Neutropenia itself may not always present clear symptoms, making it essential to monitor neutrophil counts regularly during chemotherapy. However, when symptoms do occur, they are often a result of infections. Key indicators include:
- Fever: A common symptom of CIN is an unexplained fever, often signaling an infection that the body cannot effectively fight off due to low neutrophil levels.
- Chills: Along with fever, patients may experience chills, which are also indicative of infections.
- Fatigue: Neutropenia can cause general feelings of weakness and fatigue, making everyday tasks more challenging.
- Mouth Sores: Infections in the mouth, gums, or throat can occur due to the reduced ability to fight off bacteria.
- Frequent Infections: Neutropenic patients are more susceptible to developing infections, particularly bacterial, fungal, and viral infections.
Diagnosis of Chemotherapy-Induced Neutropenia
Diagnosing CIN is based on laboratory tests and clinical observations. Key steps in diagnosing neutropenia during chemotherapy include:
- Complete Blood Count (CBC): A CBC test is the primary diagnostic tool for assessing white blood cell (WBC) levels, including neutrophils. A neutrophil count below 1,500 cells per microliter of blood is generally considered indicative of neutropenia.
- Differential Count: A breakdown of the types of white blood cells, including neutrophils, can help further assess the severity of neutropenia.
- Assessment of Infection: If a patient presents with symptoms like fever or fatigue, healthcare providers will look for signs of infection through physical exams and diagnostic imaging.
- Bone Marrow Biopsy (in severe cases): In rare situations, a bone marrow biopsy may be conducted to evaluate the marrow’s ability to produce neutrophils and rule out other causes.
Severity Classification of Chemotherapy-Induced Neutropenia
The severity of neutropenia can vary based on the patient’s neutrophil count. It is typically classified as:
- Mild Neutropenia: Neutrophil count between 1,000 and 1,500 cells per microliter of blood.
- Moderate Neutropenia: Neutrophil count between 500 and 1,000 cells per microliter of blood.
- Severe Neutropenia: Neutrophil count below 500 cells per microliter of blood.
Severe neutropenia presents the greatest risk of infections and may require immediate medical intervention to prevent life-threatening complications.
Management and Treatment of Chemotherapy-Induced Neutropenia
Managing chemotherapy-induced neutropenia involves a combination of preventive strategies, treatment modifications, and medical interventions to protect the patient’s immune system.
1. Granulocyte Colony-Stimulating Factor (G-CSF) Therapy
The primary treatment for neutropenia is the administration of granulocyte colony-stimulating factors (G-CSFs), such as filgrastim or pegfilgrastim. These medications stimulate the bone marrow to produce more neutrophils, helping to boost the patient’s immune defenses and reduce the risk of infection.
2. Adjusting Chemotherapy Regimens
In cases of severe neutropenia, chemotherapy doses may be adjusted or delayed to allow the bone marrow to recover. This approach helps reduce further bone marrow suppression and allows for the restoration of neutrophil levels.
3. Prophylactic Antibiotics
If a patient develops neutropenia, especially with a fever, prophylactic antibiotics may be prescribed to prevent infections. These antibiotics are tailored to the potential pathogens most likely to affect neutropenic individuals.
4. Infection Monitoring and Management
Close monitoring for signs of infection is essential in patients with CIN. If an infection is detected, treatment with appropriate antibiotics, antifungals, or antivirals is critical to prevent complications. In some cases, hospitalization may be required for intravenous antibiotics and intensive care.
5. Neutropenic Diet
Patients with neutropenia are often advised to follow a neutropenic diet, which limits certain foods that may carry a higher risk of bacterial contamination, such as raw or undercooked meat, seafood, and eggs. The diet also restricts unwashed fruits and vegetables to minimize exposure to harmful bacteria.
6. Hematopoietic Stem Cell Transplantation
In extreme cases where CIN is persistent and cannot be managed with standard therapies, stem cell transplantation may be considered. This approach can help re-establish normal blood cell production, although it is typically reserved for select patients.
Prevention of Chemotherapy-Induced Neutropenia
Preventing CIN is an integral part of cancer care, especially for patients receiving high-risk chemotherapy regimens. Strategies for preventing neutropenia include:
- Primary Prophylaxis with G-CSF: Administering G-CSF before or during chemotherapy can help reduce the risk of developing neutropenia.
- Dose-Scheduling Adjustments: Modifying the chemotherapy regimen or spacing out doses can help reduce the intensity of bone marrow suppression.
- Monitoring Blood Counts: Regular monitoring of blood counts before, during, and after chemotherapy allows for early detection of neutropenia and prompt intervention.
- Personalized Treatment Plans: Tailoring chemotherapy regimens based on a patient’s individual response and tolerance to drugs can reduce the likelihood of CIN.

