Chemotherapy-induced hypogonadism (CIH) represents a significant medical concern for cancer patients undergoing treatment. Hypogonadism, characterized by reduced function of the gonads (testes in men), leads to decreased production of sex hormones, including testosterone. This condition can significantly impact fertility, sexual function, and overall quality of life. Understanding its causes, symptoms, diagnostic process, and available treatment options is essential for both patients and healthcare providers.
What is Chemotherapy-Induced Hypogonadism?
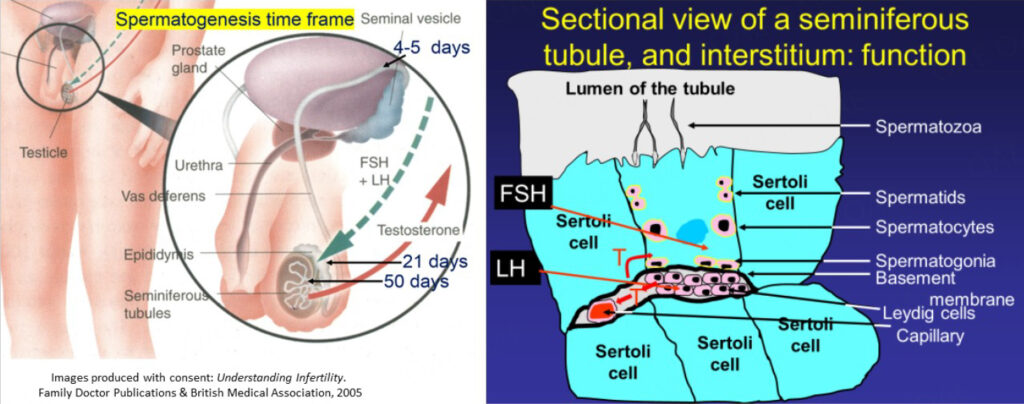
Chemotherapy-induced hypogonadism refers to the impairment of gonadal function resulting from the cytotoxic effects of chemotherapy drugs. These drugs target rapidly dividing cells, but they do not distinguish between cancerous cells and healthy cells in the body, including those in the testes. As a result, chemotherapy can damage the cells responsible for testosterone production, leading to a decrease in hormone levels and, in some cases, complete infertility.
Causes of Chemotherapy-Induced Hypogonadism
Chemotherapy drugs, while essential for treating various cancers, can have a profound impact on the endocrine system. The following are the primary factors contributing to chemotherapy-induced hypogonadism:
- Direct Testicular Toxicity: Certain chemotherapy agents, such as alkylating agents (e.g., cyclophosphamide, ifosfamide), are known to cause direct damage to the Leydig cells in the testes, responsible for testosterone production.
- Age and Pre-existing Health Conditions: The degree of gonadal damage depends on factors such as the patient’s age and pre-existing health conditions. Younger patients may experience partial recovery of testicular function, while older patients or those with additional risk factors may face permanent infertility.
- Type and Duration of Chemotherapy: The likelihood and severity of hypogonadism depend on the type, dosage, and duration of chemotherapy. High-dose regimens, especially those used in the treatment of hematologic malignancies, have a higher risk of causing permanent gonadal damage.
Symptoms of Chemotherapy-Induced Hypogonadism
The symptoms of chemotherapy-induced hypogonadism are often subtle and can develop gradually over time. Common signs include:
- Reduced Libido and Sexual Dysfunction: Testosterone plays a crucial role in sexual drive and function. A significant decline in testosterone can lead to reduced libido, erectile dysfunction, and overall sexual dissatisfaction.
- Infertility: One of the most significant concerns for male patients undergoing chemotherapy is the potential loss of fertility. Chemotherapy-induced damage to the testes may result in low sperm count or complete azoospermia (absence of sperm).
- Fatigue and Mood Changes: Low testosterone levels can contribute to fatigue, depression, and irritability, which can affect a patient’s overall well-being and quality of life.
- Loss of Muscle Mass and Bone Density: Testosterone is integral to maintaining muscle mass and bone density. Chemotherapy-induced hypogonadism can lead to muscle wasting, increased body fat, and a higher risk of osteoporosis.
- Hot Flashes and Decreased Facial Hair Growth: Similar to women experiencing menopause, men with hypogonadism may experience hot flashes and a decrease in facial and body hair growth.
Diagnosis of Chemotherapy-Induced Hypogonadism
The diagnosis of chemotherapy-induced hypogonadism typically involves a combination of patient history, clinical examination, and laboratory tests.
Hormonal Blood Tests
The primary diagnostic tool for confirming hypogonadism is measuring serum testosterone levels. A low level of testosterone, particularly in the morning when levels are highest, is indicative of hypogonadism. In addition to testosterone, other hormones such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH) may be measured to assess the functionality of the hypothalamic-pituitary-gonadal axis.
Semen Analysis
For patients concerned about fertility, a semen analysis is critical. Chemotherapy can significantly reduce sperm count and motility, and in some cases, result in permanent azoospermia.
Imaging Studies
In some cases, imaging studies such as scrotal ultrasounds may be used to rule out other potential causes of gonadal dysfunction.
Treatment Options for Chemotherapy-Induced Hypogonadism
Treatment for chemotherapy-induced hypogonadism focuses on restoring normal testosterone levels and mitigating the symptoms associated with the condition. Several approaches can be considered, depending on the severity of the condition and the patient’s fertility goals.
Hormone Replacement Therapy (HRT)
Testosterone replacement therapy (TRT) is the most common treatment for men with hypogonadism. TRT can be administered in various forms, including:
- Injectable Testosterone: Administered intramuscularly, it provides steady, long-term hormone supplementation.
- Transdermal Patches or Gels: These allow for a steady release of testosterone through the skin.
- Testosterone Implants: Small pellets implanted under the skin, offering prolonged hormone release.
While TRT can effectively manage symptoms such as low libido, fatigue, and muscle loss, it does not address fertility concerns. Therefore, for patients hoping to maintain their fertility, other options must be considered.
Fertility Preservation
For men undergoing chemotherapy who wish to preserve their fertility, sperm banking is recommended before treatment. Sperm can be collected and stored for future use in assisted reproductive technologies, such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
- Sperm Banking: The process involves the collection of sperm before starting chemotherapy, which is then frozen for later use.
- Testicular Sperm Extraction (TESE): In cases where sperm production is severely impacted, testicular sperm extraction may be used to retrieve viable sperm directly from the testes for use in fertility treatments.
Gonadotropin Therapy
In some cases, gonadotropin therapy (e.g., human chorionic gonadotropin, hCG) may be used to stimulate the testes to produce testosterone and sperm. This treatment is typically used for younger patients with partial testicular damage who are looking to preserve fertility.
Psychological Support and Counseling
The emotional toll of chemotherapy-induced hypogonadism can be significant. Psychological support and counseling are essential components of managing this condition, helping patients cope with the emotional and social consequences of sexual dysfunction, infertility, and changes in body image.
Impact on Quality of Life
Chemotherapy-induced hypogonadism can have profound effects on a patient’s quality of life. Beyond the physical symptoms, patients may experience feelings of anxiety, depression, and frustration due to the loss of fertility and sexual dysfunction. It is crucial for healthcare providers to address these issues early and offer a multidisciplinary approach, involving endocrinologists, fertility specialists, and mental health professionals, to provide comprehensive care.
Preventive Measures and Future Outlook
While chemotherapy-induced hypogonadism remains a significant concern, advances in fertility preservation techniques and hormone therapy have improved the outlook for many patients. Research into gonadal protection strategies, such as the use of gonadotropin-releasing hormone (GnRH) analogs during chemotherapy, continues to evolve.
Moreover, the development of more targeted chemotherapy agents that specifically target cancer cells while sparing healthy tissues could reduce the incidence of chemotherapy-induced hypogonadism in the future.

