Yersinia pseudotuberculosis is a Gram-negative, facultative anaerobic bacterium belonging to the Enterobacteriaceae family. It is a zoonotic pathogen, primarily affecting wild and domestic animals, but it can also cause gastrointestinal infections in humans, often resembling appendicitis or mesenteric lymphadenitis. While less prevalent than Yersinia enterocolitica, Y. pseudotuberculosis is a significant cause of enteric infections, particularly in cooler climates and during the winter season.
Etiology and Microbiological Features
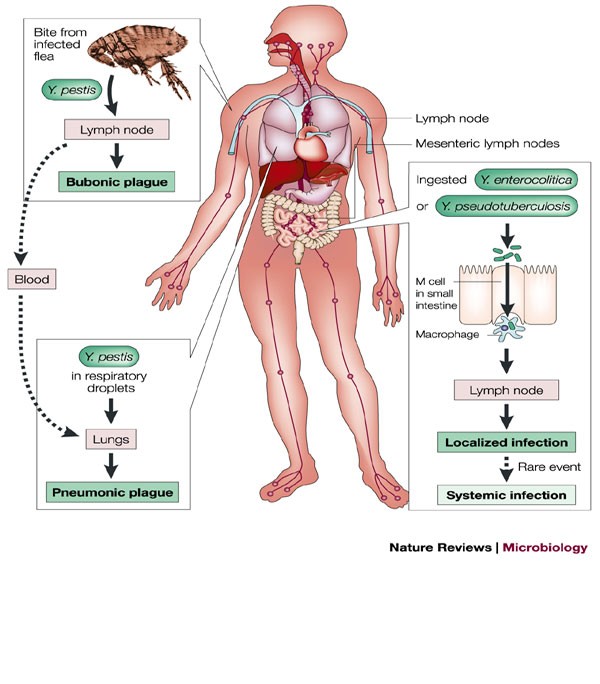
Yersinia pseudotuberculosis shares many virulence factors with its close relative Yersinia pestis (the causative agent of plague). It exhibits several pathogenic traits:
- Motile at 25°C but non-motile at 37°C
- Possesses Type III secretion systems for injecting virulence factors
- Encodes invasin (Inv) protein that facilitates penetration of the intestinal lining
- Produces Yersinia outer proteins (Yops), which interfere with immune responses
Reservoirs and Transmission Pathways
Y. pseudotuberculosis is primarily a zoonotic organism, residing in a variety of wild animals, especially rodents and birds. Domestic animals like pigs, rabbits, and livestock may also serve as reservoirs.
Common Transmission Routes:
- Fecal-oral route via contaminated food or water
- Direct contact with infected animals or their excreta
- Improperly handled meat, especially pork and game
- Unwashed fruits and vegetables grown in contaminated soil
Epidemiology and Global Prevalence
Yersinia pseudotuberculosis infections are sporadic but globally distributed, with higher prevalence in Russia, Finland, Japan, and parts of Europe. Outbreaks often occur in institutional settings like schools or military camps.
Risk Factors Include:
- Consumption of raw or undercooked meat
- Cold climate exposure
- Poor hygiene and sanitation
- Compromised immune systems
Children under 15 and elderly individuals are at higher risk of symptomatic infection.
Clinical Manifestations and Symptoms
The incubation period ranges from 5 to 10 days. Symptoms vary depending on the patient’s immune status and the site of bacterial invasion.
Common Gastrointestinal Symptoms:
- Fever
- Abdominal pain (often mimicking appendicitis)
- Diarrhea (may be bloody)
- Vomiting
- Mesenteric lymphadenitis
Systemic and Rare Complications:
- Erythema nodosum (painful red nodules on the skin)
- Reactive arthritis (especially in HLA-B27 positive individuals)
- Hepatosplenomegaly
- Septicemia in immunocompromised patients
Age-Specific Presentations:
- Children: Typically present with fever and abdominal pain
- Adults: May develop complications like arthritis and erythema nodosum
Diagnostic Approaches for Yersinia pseudotuberculosis
Accurate diagnosis is crucial due to its clinical similarity to appendicitis. Multiple laboratory techniques are employed:
Sample Collection:
- Stool cultures
- Blood cultures (in systemic cases)
- Mesenteric lymph node biopsy (if surgery is performed)
- Serological tests (ELISA or agglutination)
Laboratory Identification:
- Grows on CIN (Cefsulodin-Irgasan-Novobiocin) agar at 25°C
- Cold enrichment at 4°C enhances yield
- PCR and immunoassays can detect specific virulence genes (e.g., inv, yop, virF)
Pathogenesis of Infection
After ingestion, the bacteria colonize the ileum and Peyer’s patches, where they invade epithelial cells and evade host immune responses.
Treatment Options for Yersinia pseudotuberculosis Infection
Most infections are self-limiting, especially in immunocompetent individuals. However, in moderate to severe or systemic cases, antimicrobial therapy is recommended.
First-line Antibiotics:
- Doxycycline
- Trimethoprim-sulfamethoxazole
- Fluoroquinolones (e.g., ciprofloxacin)
- Third-generation cephalosporins (e.g., cefotaxime)
Supportive Care:
- Oral rehydration therapy
- Antipyretics
- Monitoring for complications
Avoid anti-diarrheal medications, as they may prolong the infection.
Prevention and Control Measures
To prevent Yersinia pseudotuberculosis infection, both public health measures and individual hygiene practices are crucial.
Personal and Community Preventive Strategies:
- Cook meat, especially pork, to safe temperatures
- Wash raw fruits and vegetables thoroughly
- Practice regular handwashing after animal contact
- Control rodent populations near agricultural areas
- Ensure proper sanitation in food processing environments
Veterinary and Zoonotic Considerations
Yersinia pseudotuberculosis causes enteric and systemic disease in various animals. Control in animal populations is essential to reduce human transmission.
Symptoms in Animals:
- Diarrhea
- Lethargy
- Anorexia
- Enlarged lymph nodes
- Sudden death in severe cases
Routine screening in farm environments and wildlife monitoring programs are necessary for outbreak prevention.
Public Health Surveillance and Reporting
In many countries, Yersinia infections are notifiable diseases, especially during outbreaks. Surveillance involves:
- Reporting of confirmed cases to health authorities
- Epidemiological tracing to identify contamination sources
- Environmental and food source testing
Prompt intervention can prevent large-scale foodborne outbreaks and zoonotic spillover events.
Yersinia pseudotuberculosis infection is an underrecognized but clinically significant enteric disease. Its ability to mimic appendicitis, combined with zoonotic potential and foodborne transmission, underscores the need for heightened diagnostic vigilance and public health awareness. Proper hygiene, safe food handling, and robust surveillance are key pillars in reducing the burden of this adaptable pathogen.

