Xerostomia, commonly known as dry mouth, is a condition marked by reduced or absent saliva flow. It significantly impacts oral and systemic health, leading to complications such as dental decay, oral infections, and compromised quality of life. Xerostomia is not a disease itself but a symptom of underlying conditions or treatment side effects. Its prevalence increases with age, medication use, and systemic diseases.

Saliva’s Role in Oral Health and Systemic Function
Saliva performs critical physiological roles:
- Lubricates oral tissues and aids in speech and swallowing
- Neutralizes acids, protecting dental enamel
- Contains enzymes like amylase for initiating digestion
- Offers antimicrobial protection through immunoglobulins and lysozymes
- Facilitates taste perception
A reduction in salivary flow, or hyposalivation, disrupts these functions, precipitating a cascade of oral complications.
Etiology: Common Causes of Xerostomia
Xerostomia arises from various systemic, local, and iatrogenic factors:
1. Medications
Over 500 drugs list dry mouth as a side effect. Common classes include:
- Anticholinergics
- Antihistamines
- Antidepressants (SSRIs, TCAs)
- Diuretics
- Antihypertensives
2. Systemic Diseases
- Sjögren’s syndrome: Autoimmune destruction of salivary glands
- Diabetes mellitus: Dehydration and neuropathy-related salivary gland impairment
- Parkinson’s and Alzheimer’s diseases: Autonomic dysfunction
- HIV/AIDS and Hepatitis C
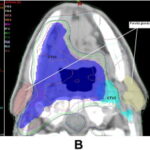
3. Cancer Therapies
- Radiotherapy to head and neck damages salivary acini
- Chemotherapy alters glandular function temporarily or permanently
4. Lifestyle and Environmental Factors
- Tobacco and alcohol use
- Caffeine intake
- Dehydration due to insufficient fluid consumption or febrile illness
- Mouth breathing, often due to nasal obstruction or sleep apnea
Recognizing Symptoms and Clinical Presentation
Common Complaints
- Persistent dry, sticky feeling in the mouth
- Difficulty in chewing, swallowing, or speaking
- Burning sensation or soreness of the tongue
- Cracked lips and angular cheilitis
- Halitosis (bad breath)
Oral Findings
- Atrophic mucosa, especially the tongue
- Cervical and root caries, especially in non-decayed patients
- Fungal infections (Candida albicans)
- Thick, ropy saliva or total lack of visible saliva
Diagnostic Evaluation of Xerostomia
1. Patient History and Symptom Index
- Medication history review
- Systemic illness and radiation exposure
- Subjective assessment using validated questionnaires like the Xerostomia Inventory
2. Sialometry
- Unstimulated whole salivary flow < 0.1 mL/min indicates hyposalivation
- Stimulated flow < 0.5 mL/min is also diagnostic
3. Sialography and Scintigraphy
- Imaging of salivary ductal system and gland function
- Essential for evaluating obstructive or structural changes
4. Lab Tests
- Autoantibody screening for Sjögren’s: Anti-SSA (Ro), Anti-SSB (La)
- Blood glucose levels, complete blood count, and viral screening when indicated
Treatment and Management of Xerostomia
1. Identify and Remove Underlying Cause
- Adjust medications where possible
- Manage systemic diseases such as diabetes or autoimmune disorders
2. Saliva Substitution and Stimulation
Pharmacological Agents
- Pilocarpine (Salagen): Muscarinic agonist
- Cevimeline (Evoxac): Selective for M3 receptors on salivary glands
- Require functional salivary tissue to be effective
Non-Pharmacological Methods
- Sugar-free lozenges, gum, and candies (xylitol-based preferred)
- Electric or gustatory stimulants
3. Saliva Substitutes
- Artificial saliva products: Mucopolysaccharide or carboxymethylcellulose-based
- Offer temporary relief, especially before meals or bedtime
4. Oral Moisturizers and Hydration
- Gels and sprays specifically formulated for dry mouth
- Frequent water sipping encouraged
Preventive Dental Measures
- Topical fluoride application
- Antibacterial rinses such as chlorhexidine for bacterial control
- Routine dental visits every 3–6 months
- Avoidance of alcohol-based mouthwashes that exacerbate dryness
- Patient education regarding sugar intake and oral hygiene
Advanced Interventions for Severe Xerostomia
- Botulinum toxin injections for hypersalivation adjustment
- Acupuncture and low-level laser therapy: Experimental but promising
- Salivary gland transfer surgery in post-radiation patients
- Stem cell and regenerative therapies under clinical trial phases
Psychosocial Impact and Quality of Life Considerations
Chronic xerostomia can cause:
- Eating and speech impairments
- Social withdrawal due to halitosis or discomfort
- Emotional distress, particularly in elderly or cancer patients
Multidisciplinary management involving dentists, rheumatologists, oncologists, and speech therapists is vital for comprehensive care.
Prognosis and Long-Term Outlook
The prognosis of xerostomia depends on the underlying cause and the effectiveness of intervention. Drug-induced cases may resolve with withdrawal or substitution. Autoimmune or radiation-related xerostomia typically requires long-term palliative care.
Continuous monitoring, patient education, and tailored therapy help mitigate complications such as rampant caries, mucosal infections, and nutritional deficiencies.
Frequently Asked Questions:
Q1: Is xerostomia reversible?
In drug-induced or transient cases, yes. Chronic autoimmune or radiation-induced xerostomia may not be reversible.
Q2: Does drinking water cure dry mouth?
Water provides temporary relief but does not stimulate salivary production. Comprehensive treatment is often necessary.
Q3: Can dry mouth increase the risk of cavities?
Yes. Saliva has protective functions. Its absence significantly increases the risk of tooth decay.
Q4: What are the best products for dry mouth relief?
Look for xylitol-based mints, saliva-stimulating gums, and artificial saliva gels or sprays.
Q5: Is xerostomia related to aging?
Aging alone does not cause xerostomia. It is often the result of medication use or underlying illness in the elderly.
Xerostomia is a multifactorial condition requiring a precise diagnostic approach and a multidisciplinary treatment strategy. Its consequences extend beyond oral discomfort, impacting systemic health, nutrition, and social well-being. Through early recognition, tailored therapeutic interventions, and preventive dental care, we can significantly improve outcomes for individuals suffering from chronic dry mouth.