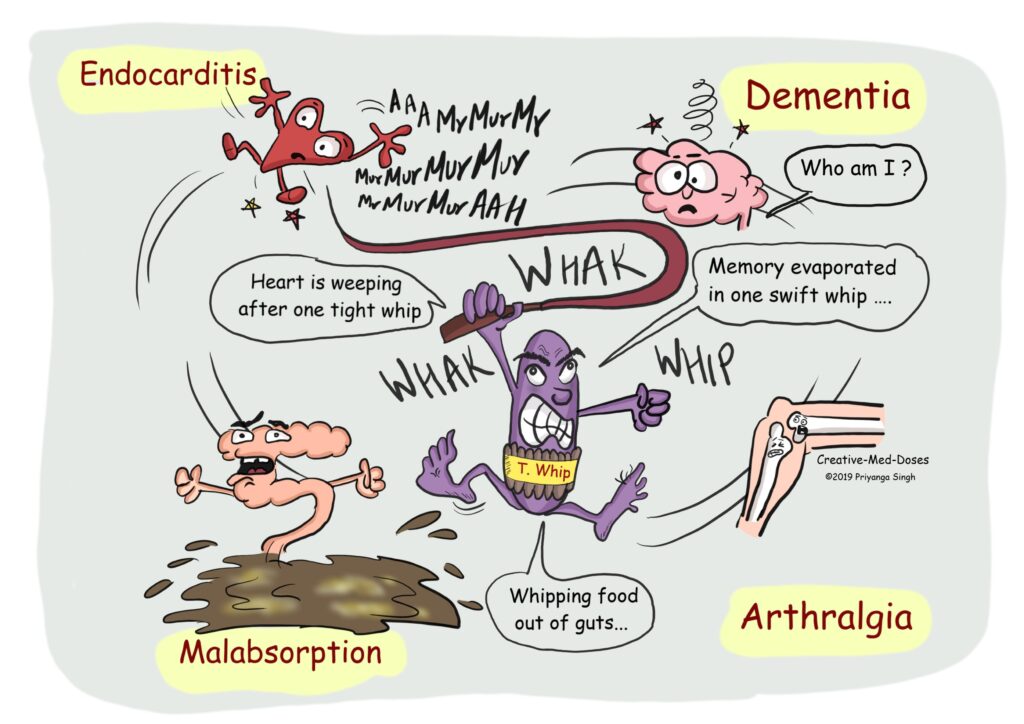
Whipple’s disease is a rare, systemic infectious disease caused by the bacterium Tropheryma whipplei. Primarily affecting the small intestine, it leads to malabsorption, but the infection can become systemic, involving multiple organs, including the heart, brain, joints, and eyes. Left untreated, it is progressively debilitating and potentially fatal.
Causative Agent: Tropheryma Whipplei
Tropheryma whipplei is a Gram-positive, rod-shaped, slow-growing bacterium. It is found in the environment and has been detected in sewage and human feces. Despite its ubiquity, disease manifestation occurs only in susceptible individuals, suggesting a role for genetic predisposition or immune dysfunction in pathogenesis.
Transmission and Risk Factors
Transmission
The exact mode of transmission remains unclear, but it is suspected to occur through the fecal-oral route. Notably, the bacterium is not considered highly contagious and is rarely transmitted from person to person.
Risk Factors
- Middle-aged Caucasian males are disproportionately affected.
- Immunocompromised individuals
- Occupational exposure to soil or wastewater
- Possible genetic predisposition impairing immune response to T. whipplei
Pathophysiology: How Whipple’s Disease Affects the Body
T. whipplei invades the lamina propria of the small intestine, resulting in villous atrophy and lymphatic obstruction, leading to fat malabsorption and systemic spread. The organism accumulates within macrophages, causing widespread inflammation in affected tissues.
Clinical Manifestations of Whipple’s Disease
The disease unfolds in phases, often beginning with nonspecific symptoms and advancing to systemic involvement.
Early Symptoms
- Arthralgia (joint pain) — may precede diagnosis by several years
- Low-grade fever
- Fatigue
- Weight loss
Gastrointestinal Symptoms
- Chronic diarrhea
- Steatorrhea (fatty stools)
- Abdominal cramping
- Malabsorption of nutrients, leading to cachexia
Systemic Symptoms
- Lymphadenopathy
- Hyperpigmentation of skin
- Cough or pleuritic pain
- Neurological symptoms (confusion, dementia, oculomotor abnormalities) in advanced cases
Diagnostic Evaluation
Clinical Suspicion
Diagnosis is often delayed due to its rarity and nonspecific presentation. A high index of suspicion is essential in individuals with unexplained weight loss, arthralgia, and chronic diarrhea.
Endoscopic and Histological Findings
- Duodenal biopsy reveals PAS-positive macrophages in the lamina propria containing T. whipplei.
- Villous blunting and lymphatic dilation are commonly observed.
Laboratory Tests
- PCR testing of tissue, cerebrospinal fluid, or stool to detect T. whipplei DNA
- Immunohistochemistry for bacterial antigens
- CBC: May show anemia and hypoalbuminemia
- CSF analysis if neurologic symptoms are present
Differential Diagnoses
- Celiac disease
- Crohn’s disease
- Intestinal lymphoma
- Tuberculosis
- HIV-related enteropathy
Each must be carefully ruled out, particularly because of overlapping symptoms like malabsorption and lymphadenopathy.
Treatment Strategy for Whipple’s Disease
Antibiotic Therapy
The cornerstone of treatment is prolonged antibiotic therapy, aimed at eradicating T. whipplei from both the intestine and systemic sites.
Initial Phase (IV therapy)
- Ceftriaxone 2 g IV daily or Meropenem for 2 weeks
Maintenance Phase (Oral therapy)
- Trimethoprim-sulfamethoxazole (TMP-SMX) for 12 months
- Alternatives: Doxycycline combined with hydroxychloroquine (for those allergic to sulfa drugs)
Monitoring and Follow-Up
- Regular clinical assessments and monitoring of symptom resolution
- PCR follow-up testing for bacterial eradication
- Neurological monitoring in patients with CNS involvement
Prognosis and Long-Term Outlook
With timely diagnosis and appropriate treatment, the prognosis is favorable, and most patients experience complete remission. However, relapse may occur, particularly in the CNS.
Poor Prognostic Indicators
- Delay in diagnosis
- Inadequate treatment duration
- CNS involvement at presentation
Complications of Untreated or Recurrent Whipple’s Disease
- Permanent neurological deficits
- Severe malnutrition and cachexia
- Cardiac complications, including endocarditis
- Fatality, especially in untreated cases
Prevention and Public Health Implications
There are currently no vaccines or prophylactic treatments. Early recognition and treatment remain the most effective strategies. Physicians should remain vigilant in patients presenting with unexplained multisystem symptoms, especially those from at-risk populations.
Whipple’s disease, though rare, is a critical differential in chronic diarrhea and systemic illness. With increasing global travel and heightened awareness, accurate and early diagnosis is now more achievable. Timely antibiotic intervention can be lifesaving, and ongoing research continues to uncover more about the immunological underpinnings of this complex bacterial infection.
Frequently Asked Questions
What is Whipple’s disease?
A rare bacterial infection caused by Tropheryma whipplei, leading to malabsorption and systemic organ involvement.
How is Whipple’s disease diagnosed?
Diagnosis is based on duodenal biopsy, PAS staining, and PCR testing for T. whipplei.
Is Whipple’s disease contagious?
No, there is no evidence of human-to-human transmission.
Can Whipple’s disease be cured?
Yes, with long-term antibiotic therapy, most patients achieve remission.
What happens if Whipple’s disease is left untreated?
It can lead to severe malabsorption, neurological impairment, and eventually death.