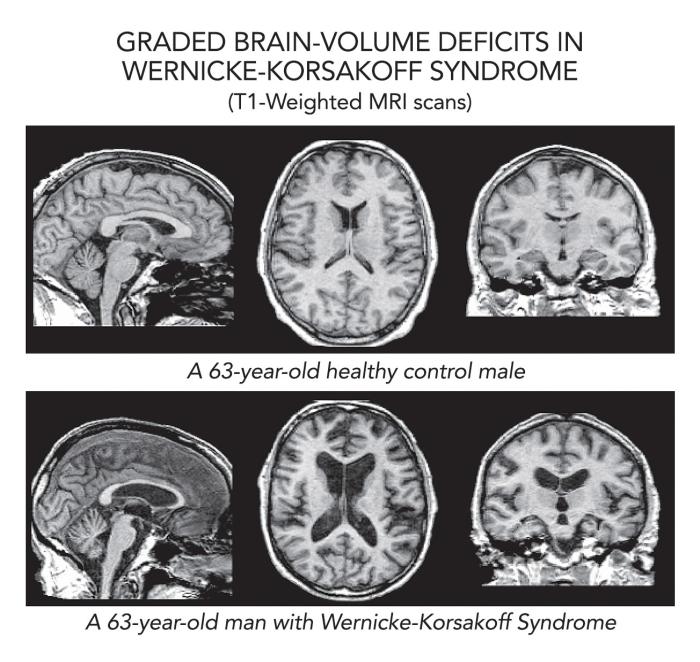
Wernicke-Korsakoff Syndrome (WKS) is a serious neurological disorder composed of two distinct but related conditions: Wernicke encephalopathy and Korsakoff psychosis. These conditions often occur sequentially due to a severe deficiency of thiamine (vitamin B1), typically linked to chronic alcohol abuse, although other causes such as malnutrition and eating disorders may contribute.
Pathophysiology of Wernicke-Korsakoff Syndrome
WKS results from impaired cerebral energy metabolism caused by thiamine deficiency. Thiamine is a vital coenzyme in glucose metabolism; its lack leads to oxidative stress, neuronal loss, and brain tissue damage, particularly in areas like the mammillary bodies, thalamus, and periaqueductal gray matter.
Causes and Risk Factors
Primary Causes
- Chronic alcohol abuse: Alcohol impairs thiamine absorption and storage.
- Severe malnutrition: Often due to anorexia nervosa, AIDS, or cancer.
- Prolonged vomiting or hyperemesis gravidarum
- Gastrointestinal surgery: Including bariatric procedures that reduce nutrient absorption.
At-Risk Populations
- Individuals with alcohol use disorder
- People with eating disorders
- Patients undergoing dialysis or chemotherapy
- Those with AIDS or liver disease
Clinical Presentation of Wernicke Encephalopathy
Wernicke encephalopathy is an acute, reversible neuropsychiatric emergency characterized by the classic triad:
- Ocular disturbances (nystagmus, ophthalmoplegia)
- Ataxia (impaired coordination)
- Confusion
In clinical practice, all three symptoms may not be present. Subtle presentations often result in missed diagnoses, which makes early intervention essential.
Progression to Korsakoff Psychosis
If Wernicke encephalopathy is left untreated, it may evolve into Korsakoff psychosis, a chronic and often irreversible syndrome. Major symptoms include:
- Anterograde and retrograde amnesia
- Confabulation (fabrication of memories)
- Executive dysfunction
- Apathy and emotional flattening
Unlike the acute phase, Korsakoff psychosis is largely irreversible and signifies lasting brain damage.
Diagnostic Evaluation
Clinical Diagnosis
- History of alcohol misuse or malnutrition
- Presence of neurological symptoms
- Response to thiamine therapy as a diagnostic trial
Imaging Techniques
- MRI of the brain: May reveal hyperintensities in the thalamus, mammillary bodies, and periaqueductal gray matter.
- CT scan: Less sensitive but can exclude other causes.
Laboratory Tests
- Serum thiamine levels: Not routinely used due to slow turnaround time.
- Liver function tests, electrolytes, and CBC to evaluate underlying conditions.
Treatment and Management
Emergency Thiamine Replacement
- IV thiamine (500 mg) three times daily for 2–3 days
- Followed by oral thiamine (100–250 mg/day) for maintenance
Important: Thiamine should be administered before any glucose infusion to avoid worsening symptoms.
Supportive Care
- Correction of electrolyte imbalances (e.g., magnesium)
- Nutritional rehabilitation
- Alcohol cessation support and addiction counseling
- Physical and occupational therapy for rehabilitation
Long-Term Prognosis
- Wernicke encephalopathy is reversible if treated early.
- Korsakoff psychosis has a guarded prognosis; approximately 25% recover fully, 50% show partial improvement, and 25% remain severely impaired.
Prevention Strategies
High-Risk Patient Monitoring
- Routine thiamine supplementation in at-risk populations
- Nutritional support in hospital settings
- Public health interventions to reduce alcohol dependency
Preventive Supplementation
- Patients with alcoholism: 100 mg/day oral thiamine
- Post-bariatric surgery patients: Long-term thiamine with multivitamins
Complications and Associated Conditions
- Peripheral neuropathy
- Cerebellar degeneration
- Delirium tremens in alcohol withdrawal
- Cognitive impairment resembling dementia
Global Prevalence and Public Health Implications
Although often underdiagnosed, WKS affects a significant percentage of chronic alcohol users, with estimates ranging from 1–2% in the general population. However, autopsy studies suggest that many cases go unrecognized. This underlines the importance of early detection and widespread awareness.
Wernicke-Korsakoff Syndrome represents a preventable yet debilitating neurological condition. Through timely diagnosis, aggressive thiamine repletion, and sustained preventive care, the irreversible complications of this disorder can be mitigated. Medical professionals must maintain a high index of suspicion in at-risk populations to ensure early intervention and optimal outcomes.
Frequently Asked Questions
What is the main cause of Wernicke-Korsakoff Syndrome?
The primary cause is thiamine (vitamin B1) deficiency, most often due to chronic alcohol consumption.
Can WKS be cured?
Wernicke encephalopathy is reversible if treated early. Korsakoff psychosis, however, often leads to permanent memory damage.
Is Wernicke-Korsakoff Syndrome hereditary?
No, it is not genetic. It results from nutritional deficiencies and lifestyle factors.
How is WKS diagnosed?
Diagnosis is clinical, supported by imaging and patient history, especially involving alcohol use or malnutrition.
How can WKS be prevented?
Routine thiamine supplementation in high-risk individuals and early nutritional support are key preventive strategies.