Adolescents with a body mass index (BMI) at or above the 95th percentile for age and sex are classified as obese. This condition poses immediate and long-term risks, including type 2 diabetes, hypertension, and psychosocial issues. Early, structured weight loss management is essential to mitigate health consequences and support healthy development. We present a multidisciplinary, evidence-based framework for treating obesity in adolescents, emphasizing individualized care.
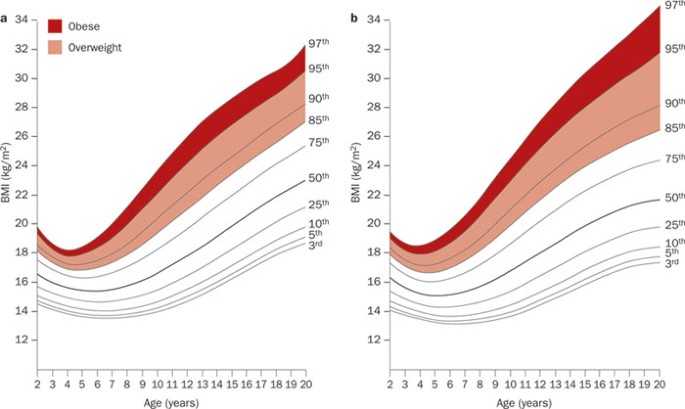
Recognizing Obesity in Adolescents by BMI Percentile
BMI percentile charts adjusted for age and sex are the gold standard for assessing adolescent weight status.
- Overweight: BMI between the 85th and 94th percentile
- Obesity: BMI ≥95th percentile
- Severe Obesity: BMI ≥120% of the 95th percentile or ≥35 kg/m² (whichever is lower)
These thresholds account for growth variations and provide a basis for clinical intervention.
Initial Assessment: Establishing the Clinical Foundation
Multidimensional Evaluation
- Anthropometric Data:
- BMI calculation and plotting on CDC/WHO growth charts
- Waist circumference to evaluate central adiposity
- Medical History & Comorbidity Screening:
- Evaluate for type 2 diabetes, dyslipidemia, NAFLD, PCOS, and hypertension
- Family history of cardiometabolic diseases
- Medication review for obesogenic drugs
- Psychosocial & Behavioral Assessment:
- Eating habits, physical activity levels, sleep patterns
- Depression, anxiety, eating disorders, screen time
- Family dynamics and socioeconomic factors
Lifestyle Modification: Core Strategy for Sustainable Weight Loss
Nutritional Counseling and Caloric Management
Nutritional intervention must focus on creating a moderate caloric deficit while maintaining essential nutrients for growth.
- Dietary Goals:
- Reduce sugar-sweetened beverages and ultra-processed foods
- Emphasize fruits, vegetables, whole grains, lean proteins
- Structured meal plans with family involvement
- Portion Control:
- Use hand-based or plate-based portion guides
- School-based meal planning and lunch packing strategies
- Professional Involvement:
- Pediatric dietitians should personalize nutrition plans considering cultural preferences and allergies
Physical Activity Prescription
Structured physical activity promotes fat loss, improves insulin sensitivity, and supports mental health.
- Target Activity Levels:
- Minimum 60 minutes/day of moderate to vigorous physical activity
- Encourage unstructured play for younger teens and sports participation for older adolescents
- Limit sedentary behavior: <2 hours/day of recreational screen time
Behavioral Therapy and Family-Based Interventions
Behavioral modification is critical to achieving and sustaining lifestyle changes.
- Motivational Interviewing:
- Enhances readiness to change and builds autonomy
- Cognitive Behavioral Therapy (CBT):
- Addresses emotional eating and negative thought patterns
- Parental Engagement:
- Whole-family behavior change leads to better outcomes
- Parents model and reinforce healthy behaviors
Medical Therapy for Adolescents with Severe Obesity or Comorbidities
When to Consider Pharmacologic Treatment
If lifestyle modifications fail after 6 months, pharmacotherapy may be considered in:
- Adolescents ≥12 years
- BMI ≥95th percentile with significant comorbidity or
- BMI ≥120% of 95th percentile without improvement through lifestyle alone
FDA-Approved Medications for Pediatric Use
| Medication | Indicated Age | Mechanism | Notes |
|---|---|---|---|
| Orlistat | ≥12 years | Lipase inhibitor | GI side effects common |
| Phentermine | ≥16 years | Appetite suppressant | Short-term use only |
| Liraglutide (Saxenda) | ≥12 years | GLP-1 receptor agonist | Injectable; also improves glycemic control |
| Semaglutide (Wegovy) | ≥12 years | GLP-1 receptor agonist | Weekly dosing, high efficacy |
- Monitoring:
- Liver enzymes, glucose, blood pressure, growth velocity
- Side effect surveillance every 3 months
Bariatric Surgery: Option for Severe Refractory Obesity
Bariatric surgery may be considered in adolescents with:
- BMI ≥35 kg/m² with major comorbidity (e.g., T2DM, OSA, NASH)
- BMI ≥40 kg/m² without comorbidities
- Failure of at least 6–12 months of lifestyle and pharmacologic therapy
Procedures commonly performed:
- Sleeve gastrectomy (most preferred in adolescents)
- Roux-en-Y gastric bypass
Postoperative Considerations:
- Long-term nutritional monitoring
- Psychological support
- Lifelong medical follow-up
Long-Term Maintenance and Relapse Prevention
Adolescent obesity is a chronic, relapsing condition requiring structured maintenance strategies:
- Regular Follow-ups: Every 3 to 6 months with a multidisciplinary team
- Peer Support & School Involvement: Support groups and active school wellness programs
- Digital Tools: Use of apps and wearable tech for tracking activity, food, and mood
- Continuous Parental Involvement: Family rules and home environment support weight stability
Addressing Socioeconomic and Cultural Barriers
Weight management must be inclusive and adaptable to individual circumstances.
- Cultural Competence: Tailor diet and activity advice to family traditions
- Access to Resources: Ensure access to safe play areas, healthy food, and affordable care
- Health Literacy: Education on food labels, cooking skills, and body image
Expected Outcomes and Clinical Goals
- Short-Term Goals (6–12 months):
- Stabilize weight or achieve 5–10% weight reduction
- Improve metabolic markers (HbA1c, ALT, lipid profile)
- Long-Term Goals:
- Normalize BMI trajectory
- Prevent adult obesity and chronic disease onset
- Improve self-esteem, academic performance, and quality of life
Frequently Asked Questions:
What BMI qualifies an adolescent for obesity treatment?
A BMI at or above the 95th percentile for age and sex qualifies an adolescent for structured obesity treatment.
How much weight should an obese adolescent lose?
A target of 5–10% reduction in body weight over 6–12 months is recommended for improving health outcomes.
Is medication safe for teens?
Yes, certain medications like liraglutide and orlistat are FDA-approved for adolescents aged 12 and older under medical supervision.
When should surgery be considered?
Bariatric surgery may be appropriate in severely obese adolescents who fail intensive non-surgical treatment and present with significant comorbidities.
Can adolescent obesity be reversed?
Yes, early intervention through multifaceted approaches can significantly reduce BMI and improve long-term health trajectories.
Weight loss management in obese adolescents—defined by BMI ≥95th percentile for age and sex—requires a structured, evidence-driven approach. A combination of nutritional planning, physical activity, behavioral therapy, pharmacologic support, and surgical evaluation forms the foundation of effective care. Long-term success hinges on family participation, psychosocial support, and ongoing monitoring to ensure healthy physical and emotional development.