A body mass index (BMI) of 27 or greater signifies a transition from overweight into the clinical zone of obesity when accompanied by comorbid conditions. At this stage, patients experience increased risks of metabolic syndrome, type 2 diabetes, cardiovascular disease, obstructive sleep apnea, and musculoskeletal disorders. Therefore, comprehensive weight loss management is not only advisable but clinically essential.
Initial Patient Assessment: Establishing a Personalized Plan
Effective management begins with a structured clinical evaluation to tailor interventions:
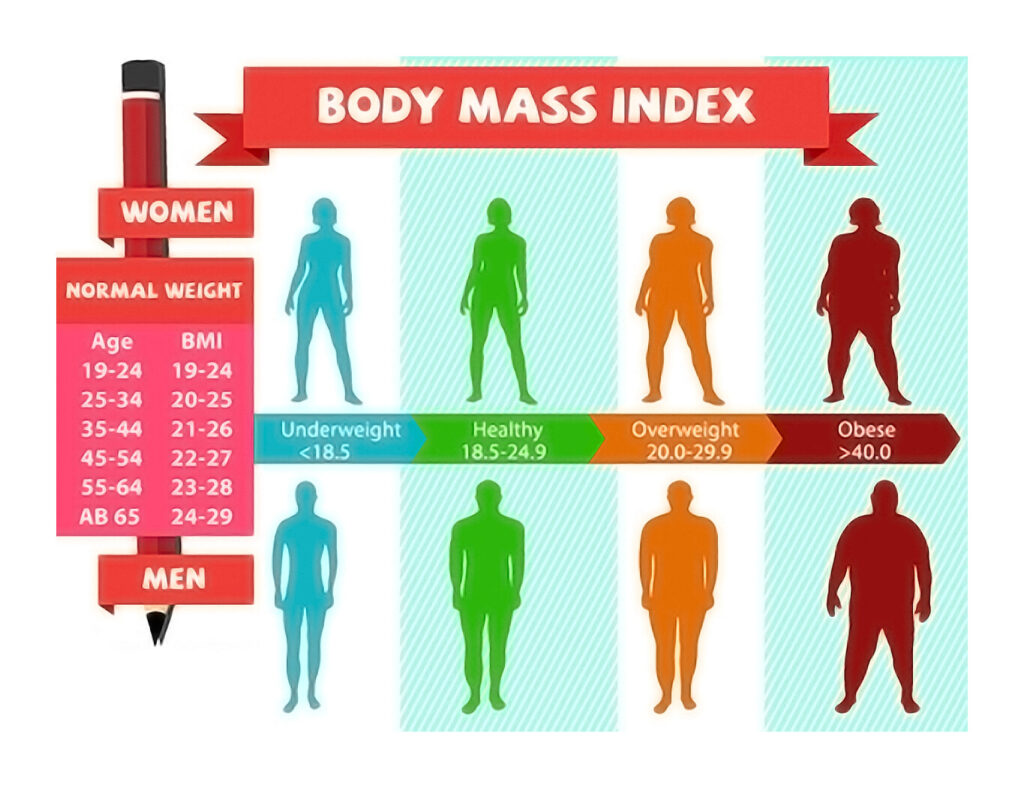
- BMI and Body Composition:
- Overweight: BMI 25.0–29.9 kg/m²
- Obese: BMI ≥30.0 kg/m²
- Use of waist circumference and body fat percentage enhances risk stratification.
- Medical and Lifestyle History:
- Review of comorbidities: hypertension, T2DM, dyslipidemia
- Dietary patterns, physical activity level, previous weight loss attempts
- Readiness to Change:
- Psychological evaluation to assess motivation, support systems, and mental health conditions such as depression or binge eating
Lifestyle Intervention: Foundation of Weight Loss Therapy
Nutritional Strategies for Sustainable Fat Loss
Structured dietary intervention remains the cornerstone of weight loss:
- Caloric Deficit Plans:
- Moderate deficit of 500–750 kcal/day supports weekly weight loss of 0.5–1.0 kg
- Typical daily intake: 1200–1500 kcal for women, 1500–1800 kcal for men
- Macronutrient Optimization:
- Emphasize high-protein, fiber-rich diets with low glycemic load
- Mediterranean and DASH diets yield strong outcomes in metabolic risk reduction
- Meal Timing and Frequency:
- Intermittent fasting and time-restricted eating may improve insulin sensitivity and promote adherence
Physical Activity Guidelines for BMI ≥27
Regular exercise enhances weight loss outcomes and preserves lean mass:
- Aerobic Exercise:
- 150–300 minutes per week of moderate-intensity activity (e.g., brisk walking, swimming)
- Resistance Training:
- 2–3 sessions per week to improve muscle mass and basal metabolic rate
- Lifestyle Movement:
- Reducing sedentary time and increasing daily steps (>10,000/day) is crucial
Behavioral Modification Techniques
- Self-Monitoring:
- Food journals, calorie tracking apps, wearable activity devices
- Goal Setting & Stimulus Control:
- SMART goals and structured environments to minimize overeating triggers
- Cognitive Behavioral Therapy (CBT):
- Identifies maladaptive behaviors, improves emotional regulation and compliance
Pharmacotherapy: Medical Management for Patients with BMI ≥27
Pharmacologic treatment is indicated in individuals with BMI ≥30, or BMI ≥27 with obesity-related comorbidities, where lifestyle changes are inadequate.
FDA-Approved Anti-Obesity Medications
| Medication | Mechanism | Suitable For |
|---|---|---|
| Orlistat | Inhibits fat absorption | Patients with high-fat diets |
| Phentermine-Topiramate | Appetite suppression, satiety increase | Long-term weight loss maintenance |
| Naltrexone-Bupropion | Reduces cravings and emotional eating | Binge eating or food addiction |
| Liraglutide (3.0 mg) | GLP-1 receptor agonist | Diabetics with cardiovascular risks |
| Semaglutide (2.4 mg) | GLP-1 receptor agonist | High efficacy with weekly dosing |
Medication Monitoring and Response
Treatment should yield ≥5% weight loss within 12 weeks to continue. Regular lab monitoring and follow-up visits assess safety, adherence, and clinical response.
Surgical Interventions for Advanced Obesity
In cases where BMI ≥35 with comorbidities or BMI ≥40, and other methods fail, bariatric surgery becomes the most effective intervention.
Bariatric Procedures
- Sleeve Gastrectomy:
- Restrictive; lowers ghrelin levels and enhances early satiety
- Roux-en-Y Gastric Bypass:
- Both restrictive and malabsorptive; effective for diabetes remission
- Adjustable Gastric Banding:
- Now less commonly used due to lower efficacy and higher complication rates
Benefits and Considerations
- Long-term weight loss of 25–35% of initial weight
- Improvement or remission of T2DM, sleep apnea, and cardiovascular risks
- Requires ongoing nutritional support and psychological counseling
Monitoring Progress and Ensuring Long-Term Success
Weight loss maintenance requires structured, ongoing care to prevent weight regain and support metabolic stability.
Follow-Up Frequency
- Monthly visits during initial 6–12 months
- Quarterly evaluations thereafter
- Review of weight trends, labs, medication side effects, and mental health
Maintenance Techniques
- Continued use of food/activity logs
- Flexible dietary plans with reintroduction of variety
- Periodic behavioral therapy sessions
Addressing Psychosocial and Environmental Influences
Management must address broader determinants:
- Mental Health Integration:
- Treatment for depression, anxiety, and eating disorders
- Cultural Sensitivity:
- Tailoring strategies to food customs, socioeconomic status, and literacy
- Environmental Support:
- Access to parks, healthy foods, and fitness resources improves outcomes
Frequently Asked Questions:
What is the goal weight loss percentage for BMI ≥27?
A 5–10% reduction in body weight improves blood pressure, lipid levels, and glucose tolerance significantly.
Are medications necessary for patients with BMI 27?
If comorbidities exist and lifestyle interventions alone fail, medications are appropriate and often essential.
Is surgery an option for overweight patients?
Not typically. Surgery is reserved for BMI ≥35 with conditions or BMI ≥40 after conservative measures have failed.
How quickly should weight loss occur?
A safe target is 0.5–1 kg per week, achieved via caloric deficit and activity increase without rapid or extreme dieting.
Can patients regain weight after initial success?
Yes. Weight regain is common without sustained lifestyle change and follow-up. Structured maintenance reduces this risk.
Weight loss management for overweight and obese patients with BMI ≥27 demands a multifaceted, personalized approach. Integrating nutritional changes, physical activity, behavior modification, pharmacotherapy, and surgical options—where indicated—yields optimal outcomes. Continuous engagement, medical oversight, and supportive environments are critical for long-term success and disease risk reduction.

