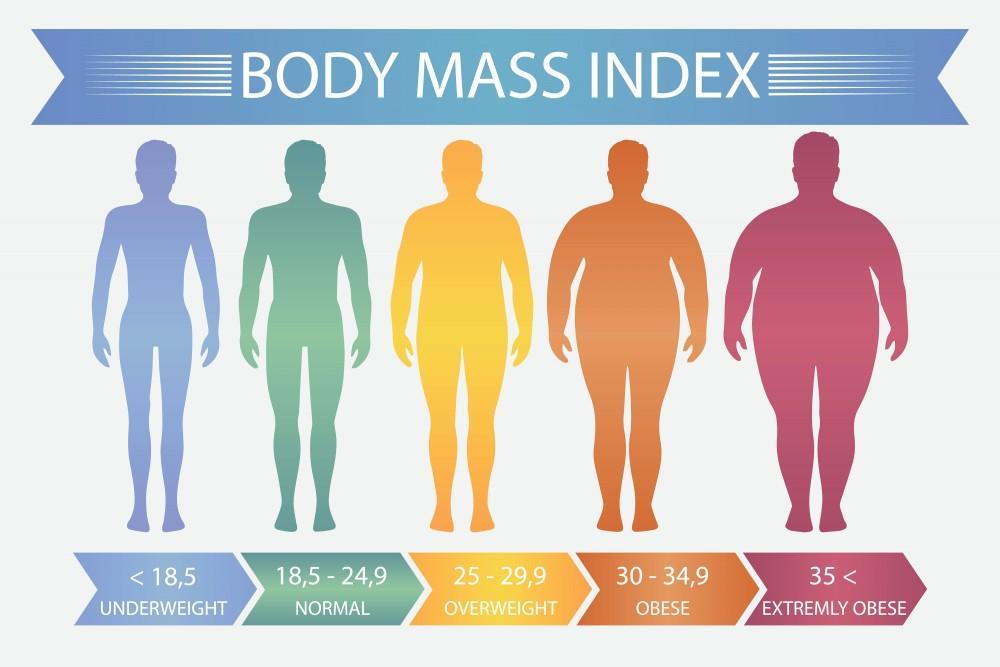
Obesity, defined as a body mass index (BMI) of 30 or greater, is a chronic, multifactorial disease with serious health consequences including type 2 diabetes, cardiovascular disease, sleep apnea, osteoarthritis, and certain cancers. Effective weight loss management for obese patients necessitates a structured, personalized, and sustainable approach that targets the underlying causes while incorporating lifestyle, pharmacologic, and surgical interventions.
Comprehensive Assessment in Obese Patients
A successful weight management plan begins with a thorough evaluation:
- BMI Classification:
- Class I Obesity: 30.0–34.9 kg/m²
- Class II Obesity: 35.0–39.9 kg/m²
- Class III Obesity (Severe): ≥40.0 kg/m²
- Waist Circumference:
- A key marker of visceral adiposity; increased risk if >102 cm in men or >88 cm in women.
- Comorbidity Evaluation:
- Hypertension, insulin resistance, dyslipidemia, NAFLD, PCOS, depression.
- Lifestyle and Dietary Patterns:
- Caloric intake, eating behaviors, physical activity, psychosocial factors.
Evidence-Based Lifestyle Modifications for Obesity Management
Behavioral lifestyle changes form the cornerstone of obesity treatment. A caloric deficit of 500–1000 kcal/day typically yields a weekly weight loss of 0.5–1 kg.
Nutrition Therapy:
- Hypocaloric Diets:
- 1200–1500 kcal/day for women
- 1500–1800 kcal/day for men
- Macronutrient Composition:
- High-protein, low-glycemic index foods improve satiety and glucose control.
- Meal Replacements & Structured Plans:
- Proven effective for initiating weight loss in clinical settings.
Physical Activity:
- 150–300 minutes/week of moderate-intensity aerobic exercise recommended.
- Resistance training 2–3 times/week enhances fat loss and muscle preservation.
- Movement throughout the day counters sedentary behavior.
Behavioral Therapy:
- Cognitive-behavioral interventions improve adherence.
- Self-monitoring via food diaries and activity logs.
- Regular counseling with dietitians or certified health coaches.
Pharmacological Therapy: Medical Options for Patients with BMI ≥30
When lifestyle modifications alone are insufficient, anti-obesity medications may be prescribed for individuals with BMI ≥30, or BMI ≥27 with obesity-related conditions.
Approved Medications:
| Drug | Mechanism | Common Side Effects |
|---|---|---|
| Orlistat | Lipase inhibitor | GI discomfort, oily stools |
| Phentermine-topiramate | Appetite suppressant & antiepileptic | Insomnia, dry mouth |
| Naltrexone-bupropion | Dopamine/norepinephrine modulation | Nausea, constipation |
| Liraglutide (GLP-1) | Appetite suppression, delayed gastric emptying | Nausea, vomiting |
| Semaglutide (GLP-1) | Enhances satiety, reduces intake | GI symptoms, pancreatitis risk |
Pharmacotherapy should be adjunctive to lifestyle interventions, and therapy continuation must be re-evaluated after 12 weeks to assess efficacy.
Bariatric Surgery: An Effective Option for Severe Obesity
For patients with BMI ≥40 or BMI ≥35 with serious comorbidities, bariatric surgery offers the most substantial and sustained weight loss outcomes.
Common Procedures:
- Roux-en-Y Gastric Bypass (RYGB):
- Alters digestive anatomy; hormonal and restrictive effects.
- Sleeve Gastrectomy:
- Removes a portion of the stomach; reduces ghrelin production.
- Adjustable Gastric Banding (less commonly used):
- Involves band placement to restrict food intake.
Outcomes:
- Average loss of 25–35% of baseline weight within 1–2 years.
- Substantial improvements in diabetes remission, blood pressure, and lipid profiles.
Bariatric procedures require lifelong follow-up, nutritional supplementation, and psychological support.
Monitoring and Long-Term Maintenance of Weight Loss
Sustained weight loss requires continuous care and structured follow-up. Many patients regain a portion of lost weight due to metabolic adaptations and behavioral relapse.
Long-Term Strategies:
- Monthly or quarterly clinical follow-ups.
- Ongoing dietary adjustments and psychological support.
- Continued physical activity and self-monitoring.
- Medication or surgical re-evaluation if weight regain occurs.
Goals:
- Prevent weight regain ≥5% of body weight.
- Maintain metabolic and functional improvements.
- Reduce morbidity and improve quality of life.
Psychosocial and Environmental Considerations
Obesity is influenced by socioeconomic status, cultural factors, food environment, and mental health. These must be addressed within the management plan.
- Mental Health Screening:
- Treat depression, anxiety, and eating disorders.
- Community Support Programs:
- Group counseling, obesity support groups.
- Workplace and School Interventions:
- Encouraging physical activity and healthy food choices.
Frequently Asked Questions:
What is the best first step in weight loss for a BMI over 30?
The first step is a medically supervised plan focusing on dietary change, increased activity, and behavioral strategies.
How much weight loss is clinically meaningful?
Losing 5–10% of body weight significantly improves blood sugar, blood pressure, and lipid levels.
When should medications be added for obesity?
If after 3–6 months of lifestyle changes there is <5% weight loss and the BMI remains ≥30 (or ≥27 with comorbidities), pharmacotherapy is indicated.
Is bariatric surgery safe for all obese patients?
Surgery is generally safe but recommended only after a comprehensive evaluation and failure of non-invasive measures.
Can weight regain be prevented?
Yes, with structured maintenance plans, continued support, and periodic re-assessment of behavioral and metabolic factors.
Effective weight loss management for obese patients with BMI 30 or greater requires a multimodal strategy encompassing lifestyle modification, medical therapy, and potentially surgery. A tailored, evidence-based plan—supported by interdisciplinary teams—yields sustainable results, mitigates complications, and enhances overall health outcomes. Long-term success hinges on patient engagement, continuous support, and regular monitoring.