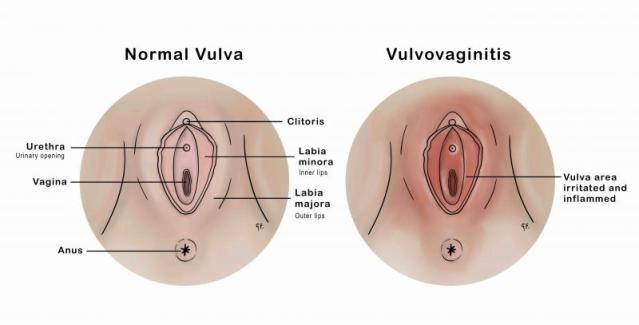
Vulvovaginitis refers to the inflammation of the vulva and vagina, resulting from infections, irritants, allergens, or systemic conditions. It is a broad clinical term encompassing several etiologies and presents across all age groups—from prepubescent children to postmenopausal women. The condition remains one of the most common gynecological complaints, characterized by discomfort, abnormal discharge, odor, and itching.
Classification of Vulvovaginitis Based on Cause
Infectious Causes:
- Bacterial Vaginosis (BV): Overgrowth of anaerobic bacteria replacing normal Lactobacillus
- Vulvovaginal Candidiasis (VVC): Fungal infection by Candida albicans
- Trichomoniasis: Protozoal sexually transmitted infection
Non-Infectious Causes:
- Allergic/Irritant Dermatitis: Soaps, perfumes, sanitary products
- Atrophic Vaginitis: Postmenopausal estrogen deficiency
- Foreign Body-Induced: Retained tampons, toilet paper in children
- Systemic Diseases: Diabetes, autoimmune disorders
Common Symptoms of Vulvovaginitis
Symptoms vary by etiology but generally include:
- Vaginal itching or burning
- Abnormal vaginal discharge (color, odor, consistency)
- Dysuria (painful urination)
- Dyspareunia (painful intercourse)
- Vulvar erythema, edema, or ulceration
- Vaginal bleeding (occasionally in atrophic or erosive cases)
In pediatric cases, symptoms may also include behavioral changes, genital discomfort, and increased urinary frequency.
Bacterial Vaginosis: The Leading Cause of Vulvovaginitis
Bacterial vaginosis (BV) is the most common cause in reproductive-aged women. It results from the disruption of normal vaginal flora, allowing anaerobic organisms like Gardnerella vaginalis to proliferate.
Key Indicators:
- Thin, gray-white homogeneous discharge
- Fishy odor, especially post-intercourse (positive “whiff test”)
- Vaginal pH > 4.5
- Clue cells on wet mount microscopy
Recommended Treatment:
- Metronidazole 500 mg orally twice daily for 7 days
- Clindamycin 2% vaginal cream at bedtime for 7 days
- Avoid alcohol during and after metronidazole therapy
Vulvovaginal Candidiasis: Fungal Origin of Vaginitis
Often caused by Candida albicans, this infection is characterized by:
- Thick, white, curd-like discharge
- Intense itching and burning
- Red, swollen vulvar tissue
- Normal vaginal pH (< 4.5)
Standard Treatment:
- Fluconazole 150 mg orally (single dose)
- Topical antifungals: clotrimazole, miconazole for 3–7 days
- For recurrent cases (≥4/year), maintenance therapy is essential
Trichomoniasis: Protozoal Sexually Transmitted Cause
Caused by Trichomonas vaginalis, this form presents with:
- Frothy, yellow-green discharge
- Strong, unpleasant odor
- Vulvar irritation
- Strawberry cervix (petechiae)
Treatment Protocol:
- Metronidazole 2 g orally in a single dose
- Treat all sexual partners simultaneously
- Abstain from sexual activity until symptoms resolve
Non-Infectious Vulvovaginitis: Irritant and Allergic Etiologies
Vaginal inflammation is not always infectious. Common triggers include:
- Scented hygiene products
- Douches
- Tight-fitting synthetic clothing
- Laundry detergents
Clinical Signs:
- Redness without discharge
- Burning, itching
- Often recurrent with repeated exposure
Management:
- Eliminate irritants
- Use mild, hypoallergenic cleansers
- Apply topical corticosteroids (low-potency) in severe cases
Atrophic Vaginitis in Postmenopausal Women
Also known as genitourinary syndrome of menopause (GSM), it results from estrogen deficiency.
Symptoms:
- Vaginal dryness
- Dyspareunia
- Burning or itching
- Urinary symptoms (frequency, urgency, dysuria)
Treatment:
- Vaginal estrogen therapy: creams, rings, tablets
- Non-hormonal moisturizers and lubricants
- Oral selective estrogen receptor modulators (SERMs) in select cases
Pediatric Vulvovaginitis: A Distinct Clinical Entity
In prepubertal girls, thin vulvar skin and lack of estrogen make them prone to irritation and infections.
Common Causes:
- Poor hygiene
- Bubble baths, soaps
- Pinworms
- Foreign bodies
Treatment Approach:
- Gentle cleaning with water
- Cotton underwear, avoidance of irritants
- Antibiotics if bacterial infection is confirmed
- Rule out abuse in recurrent or unexplained cases
Diagnostic Workup of Vulvovaginitis
Accurate diagnosis is essential for effective treatment. It involves:
- Detailed history and physical examination
- pH testing (normal < 4.5; elevated in BV and trichomoniasis)
- Wet mount microscopy (saline and KOH prep)
- Vaginal swabs for Gram stain or NAAT (Nucleic Acid Amplification Testing)
- Fungal cultures or bacterial cultures in refractory cases
Preventive Measures for Vulvovaginitis
- Maintain vaginal pH and flora with appropriate hygiene
- Avoid douching and scented products
- Practice safe sex; use condoms
- Probiotics may aid in flora restoration post-antibiotics
- Regular gynecological check-ups, especially for high-risk individuals
When to Seek Medical Attention
Immediate consultation is advised if:
- Symptoms persist despite home treatment
- Vaginal discharge is bloody or foul-smelling
- There is fever or systemic illness
- Pain or ulcers develop in the vulvovaginal region
- Vulvovaginitis recurs frequently or affects daily function
Vulvovaginitis represents a spectrum of conditions with varied causes, presentations, and treatments. Accurate classification and targeted management are vital to relieve symptoms, prevent recurrence, and restore vaginal health. By maintaining hygiene, avoiding known triggers, and consulting healthcare professionals early, we can effectively manage this common but often distressing condition.