Vulvovaginal candidiasis (VVC), commonly referred to as a vaginal yeast infection, is a fungal infection of the vulva and vagina, predominantly caused by Candida albicans. It is one of the most frequent gynecological conditions, affecting up to 75% of women at least once in their lifetime. Although generally not life-threatening, VVC significantly impacts quality of life due to discomfort and recurrent episodes.
Causes and Pathophysiology of Vaginal Yeast Infections
VVC occurs when there is an overgrowth of Candida species, particularly Candida albicans, which is normally part of the vaginal flora. Disruption in the vaginal microenvironment allows the yeast to proliferate and invade the mucosal tissue.
Primary Contributing Factors:
- Antibiotic Use: Disruption of lactobacilli and normal flora
- High Estrogen Levels: Pregnancy, oral contraceptives, hormone replacement therapy
- Immunosuppression: HIV, corticosteroid therapy, diabetes mellitus
- Tight or Non-Breathable Clothing: Creates a warm, moist environment
- Douching or Vaginal Products: Alters pH and disrupts microbial balance
Classification of Vulvovaginal Candidiasis
VVC is categorized based on the frequency and severity of symptoms, as well as the response to treatment.
1. Uncomplicated VVC:
- Sporadic or infrequent episodes
- Mild to moderate symptoms
- Candida albicans involvement
- Healthy, non-pregnant women
2. Complicated VVC:
- Severe symptoms (edema, excoriation, fissures)
- Recurrent episodes (≥4/year)
- Non-albicans Candida species (e.g., Candida glabrata)
- Pregnancy or immunosuppressed patients
Symptoms of Vulvovaginal Candidiasis
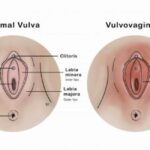
The clinical presentation of VVC varies depending on the severity and type of infection.
Common Symptoms:
- Intense vulvovaginal itching or burning
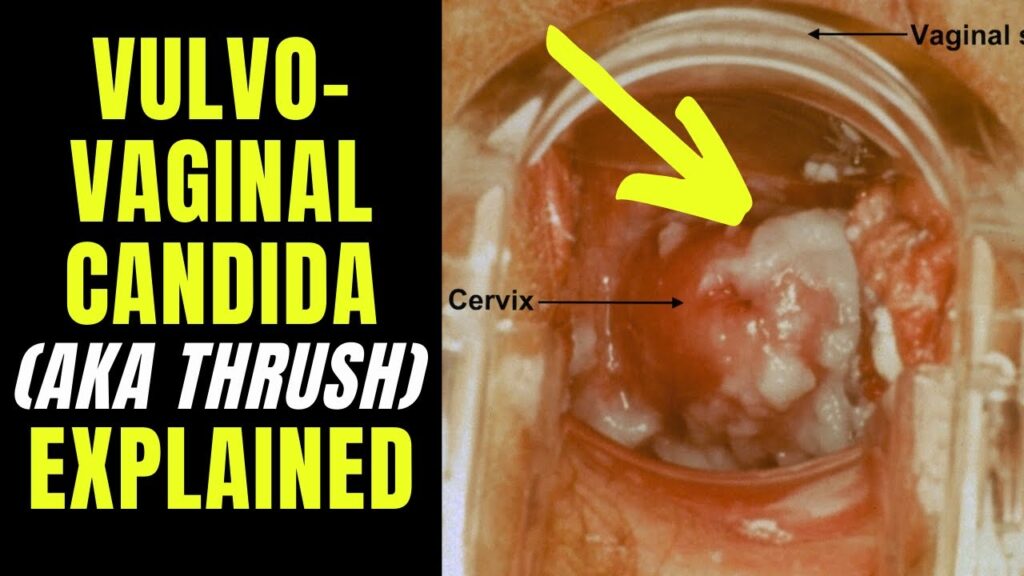
- Thick, white, “cottage cheese-like” vaginal discharge
- Erythema, edema, or fissures of vulvar tissue
- Dysuria (pain during urination)
- Dyspareunia (painful intercourse)
In recurrent or chronic cases, psychological effects such as anxiety or sexual dysfunction may also develop due to persistent discomfort.
Diagnostic Approach to Vaginal Yeast Infections
Accurate diagnosis is essential to distinguish VVC from other causes of vaginitis, such as bacterial vaginosis or trichomoniasis.
Diagnostic Tools:
- History and Physical Examination: Assessment of clinical signs and risk factors
- Vaginal pH Testing: VVC typically maintains a normal vaginal pH (<4.5)
- Microscopy (Wet Mount/KOH Prep): Identifies budding yeast, pseudohyphae
- Culture or PCR Testing: Especially useful in recurrent or treatment-resistant cases
- Gram Stain: Confirms yeast presence and estimates microbial load
Treatment Strategies for Vulvovaginal Candidiasis
1. Antifungal Therapy
a. Topical Agents (Intravaginal):
- Clotrimazole 1% or 2% Cream
- Miconazole Suppositories
- Tioconazole Ointment
- Duration: 1 to 7 days depending on the formulation
b. Oral Agents:
- Fluconazole 150 mg: Single-dose oral tablet
- Itraconazole: Alternative in fluconazole-resistant cases
Note: Oral antifungals are contraindicated during pregnancy; topical treatment is preferred.
2. Treatment of Complicated VVC:
- Extended Therapy: Fluconazole on days 1, 4, and 7
- Maintenance Regimen: Weekly fluconazole for 6 months (for recurrent VVC)
- Non-Albicans Infections: May require topical boric acid (600 mg intravaginally for 14 days)
Managing Recurrent Vulvovaginal Candidiasis (RVVC)
RVVC, defined as four or more episodes in a year, often results from incomplete eradication, reinfection, or an underlying host susceptibility.
Management Protocol:
- Induction Therapy: Oral fluconazole or topical antifungals for initial control
- Maintenance Therapy: Oral fluconazole 150 mg once weekly for six months
- Boric Acid or Nystatin Suppositories: For azole-resistant strains
- Lifestyle Modifications: Avoid tight clothing, douching, perfumed products
Prevention and Risk Reduction Measures
Lifestyle and Behavioral Modifications:
- Wear cotton underwear and avoid moisture-retaining clothing
- Avoid unnecessary antibiotic use
- Maintain proper genital hygiene without harsh soaps or douching
- Control underlying diabetes and other chronic conditions
Probiotic Use:
- Oral or vaginal probiotics containing Lactobacillus may help restore normal flora and reduce recurrence, though evidence remains inconclusive.
Vulvovaginal Candidiasis in Special Populations
Pregnancy:
- More susceptible due to elevated estrogen and glycogen
- Only topical antifungals are recommended (e.g., clotrimazole, miconazole)
Diabetics:
- Higher risk of chronic and severe VVC
- Require tighter glycemic control and may need prolonged therapy
Immunocompromised Individuals:
- At risk for atypical and refractory infections
- May need individualized, aggressive antifungal management
Potential Complications if Left Untreated
While VVC is not life-threatening, untreated infections can result in:
- Chronic inflammation and scarring
- Vulvar dermatitis and secondary bacterial infections
- Negative impact on sexual and psychological well-being
- Rare progression to invasive candidiasis in immunocompromised individuals
Vulvovaginal candidiasis is a common, often recurrent, fungal infection that can significantly affect a woman’s health and quality of life. Timely diagnosis, tailored antifungal therapy, and preventive strategies are key to effective management. By addressing both microbial and host-related factors, we can minimize recurrence and complications, ensuring optimal reproductive health outcomes.