Vitamin K is a fat-soluble nutrient critical for blood clotting, bone metabolism, and cardiovascular health. Due to its fat-soluble nature, absorption of vitamin K depends heavily on proper digestion and assimilation of dietary fats. Any disruption in fat absorption—whether from gastrointestinal disorders, liver dysfunction, or surgical interventions—can impair vitamin K uptake and lead to deficiency.
The Role of Vitamin K in Human Physiology
Vitamin K exists in two primary forms:
- Phylloquinone (Vitamin K1): Found in green leafy vegetables
- Menaquinones (Vitamin K2): Produced by gut microbiota and found in fermented foods
Both forms contribute to:
- Activation of clotting factors II, VII, IX, and X, and proteins C and S
- Regulation of osteocalcin for bone mineralization
- Inhibition of vascular calcification
Without adequate vitamin K, the body cannot properly form clots, increasing the risk of excessive bleeding.
Causes of Vitamin K Deficiency Due to Fat Malabsorption
1. Chronic Fat Malabsorption Syndromes
Conditions that impair digestion and absorption of fats inevitably reduce vitamin K assimilation. These include:
- Cystic fibrosis
- Celiac disease
- Crohn’s disease
- Chronic pancreatitis
- Short bowel syndrome
2. Hepatobiliary Disorders
Vitamin K absorption requires bile acids to emulsify fats. Disorders affecting bile production or flow reduce absorption:
- Primary biliary cholangitis
- Obstructive jaundice
- Liver cirrhosis
3. Long-Term Use of Certain Medications
- Antibiotics (disrupt gut flora responsible for K2 synthesis)
- Cholestyramine and orlistat (interfere with fat absorption)
- Anticoagulants like warfarin (antagonize vitamin K activity)
4. Total Parenteral Nutrition (TPN) Without Adequate Supplementation
Patients on TPN for extended periods without proper vitamin K inclusion are at risk of deficiency.
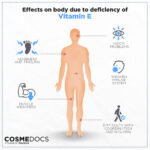
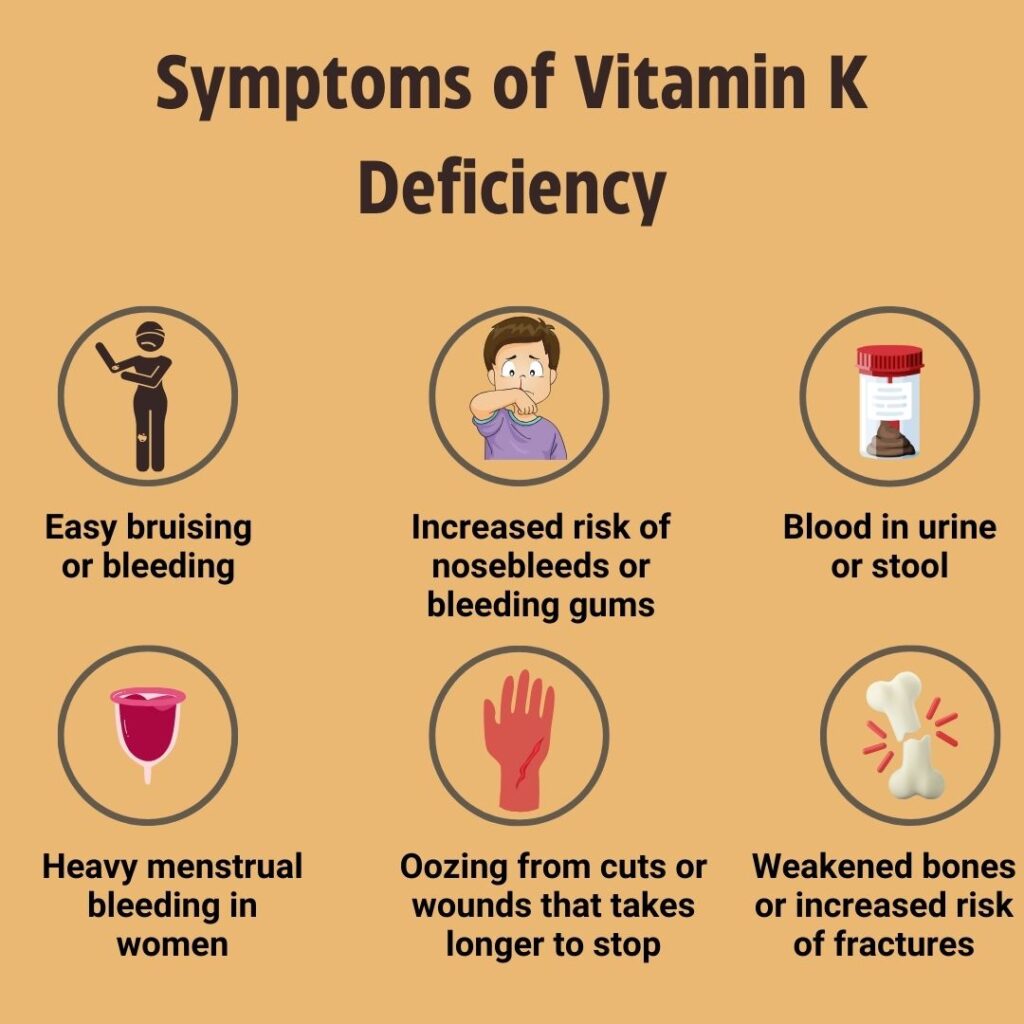
Clinical Manifestations of Vitamin K Deficiency
Deficiency results in impaired synthesis of coagulation factors, leading to:
- Easy bruising
- Prolonged bleeding from wounds or surgical sites
- Hematuria (blood in urine)
- Melena (black tarry stools)
- Menorrhagia (heavy menstrual bleeding)
- Intracranial hemorrhage in severe neonatal deficiency
In newborns, the condition may present as Vitamin K Deficiency Bleeding (VKDB), formerly known as hemorrhagic disease of the newborn.
Diagnostic Evaluation
1. Prothrombin Time (PT)
- The most sensitive indicator of vitamin K deficiency
- Prolonged PT with normal activated partial thromboplastin time (aPTT) indicates early deficiency
2. Serum Vitamin K Levels
- Direct measurement is possible but not routinely used due to high cost and variability
3. PIVKA-II Test (Proteins Induced by Vitamin K Absence)
- Detects abnormal, under-carboxylated prothrombin
- Useful in identifying subclinical deficiency
4. Stool Fat Analysis
- Confirms fat malabsorption as an underlying etiology
Dietary and Clinical Sources of Vitamin K
Incorporating vitamin K-rich foods is essential in both prevention and management.
| Food Source | Vitamin K Content (µg per 100g) |
|---|---|
| Kale | 817 µg |
| Spinach | 483 µg |
| Broccoli | 101 µg |
| Brussels sprouts | 140 µg |
| Natto (fermented soy) | 1103 µg (K2) |
| Egg yolk | 34 µg |
| Liver (beef/chicken) | 106 µg |
Treatment Strategies
1. Vitamin K Supplementation
- Oral supplementation is sufficient in mild cases: 1–10 mg/day
- Parenteral administration (IV or IM): Used in severe or acute deficiency, particularly in bleeding episodes
- In neonates, prophylactic injection of 0.5–1 mg vitamin K1 at birth is standard
2. Managing Underlying Malabsorption
- Treating the root cause—be it inflammatory bowel disease, liver dysfunction, or enzyme insufficiency—is essential for long-term correction
3. Fat-Soluble Vitamin Formulations
- For chronic conditions like cystic fibrosis, water-miscible forms of vitamin K improve absorption
- Multivitamin regimens with added vitamins A, D, E, and K are often prescribed
Preventive Measures for At-Risk Populations
- Regular monitoring of coagulation parameters in patients with fat malabsorption
- Neonatal prophylaxis for all infants, especially those born prematurely
- Vitamin K supplementation during long-term antibiotic use or TPN
- Dietary counseling to ensure sufficient intake of leafy greens and fermented foods
Long-Term Consequences of Untreated Deficiency
Persistent vitamin K deficiency due to malabsorption can result in:
- Chronic bleeding diathesis
- Anemia secondary to blood loss
- Increased risk of osteoporosis and arterial calcification
- Severe neonatal hemorrhage if not promptly addressed
In patients undergoing surgery, even subclinical deficiency can cause significant intraoperative bleeding complications.
Vitamin K deficiency due to fat malabsorption represents a clinically significant issue requiring timely recognition, diagnostic precision, and targeted treatment. By understanding the critical interplay between fat digestion and vitamin K absorption, we can more effectively manage and prevent this condition. Early intervention, dietary optimization, and monitoring of high-risk individuals form the cornerstone of successful long-term outcomes.