Ventricular tachycardia (VT) is a potentially life-threatening cardiac arrhythmia originating from the ventricles, defined by a heart rate exceeding 100 beats per minute and typically presenting with three or more consecutive ventricular beats. Its prompt identification and management are critical, especially in structurally abnormal hearts.
Types of Ventricular Tachycardia
Monomorphic Ventricular Tachycardia
This form displays uniform QRS complexes on an ECG, suggesting a stable, singular focus of arrhythmic origin. It often arises from structural heart disease, particularly post-myocardial infarction scarring.
Polymorphic Ventricular Tachycardia
Characterized by varying QRS morphologies, polymorphic VT is often associated with acute ischemia, electrolyte imbalance, or prolonged QT interval. Torsades de Pointes is a notable subtype that may rapidly degenerate into ventricular fibrillation.
Underlying Causes of Ventricular Tachycardia
Structural Heart Disease
- Ischemic cardiomyopathy: Scar tissue post-MI often acts as a re-entry circuit.
- Non-ischemic cardiomyopathy: Includes dilated or hypertrophic variants.
- Valvular heart disease: Aortic stenosis and mitral valve prolapse are contributors.
Non-Structural Etiologies
- Electrolyte disturbances: Hypokalemia, hypomagnesemia.
- Drug toxicity: Especially class I and III antiarrhythmics, digoxin.
- Congenital syndromes: Long QT, Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy (ARVC).
Clinical Presentation of Ventricular Tachycardia
Symptoms vary based on duration, rate, and cardiac function. Common presentations include:
- Palpitations
- Dizziness or presyncope
- Syncope
- Chest pain
- Dyspnea
- Sudden cardiac arrest (in sustained VT)
Hemodynamic instability is a critical determinant of urgency in management.
Diagnostic Evaluation
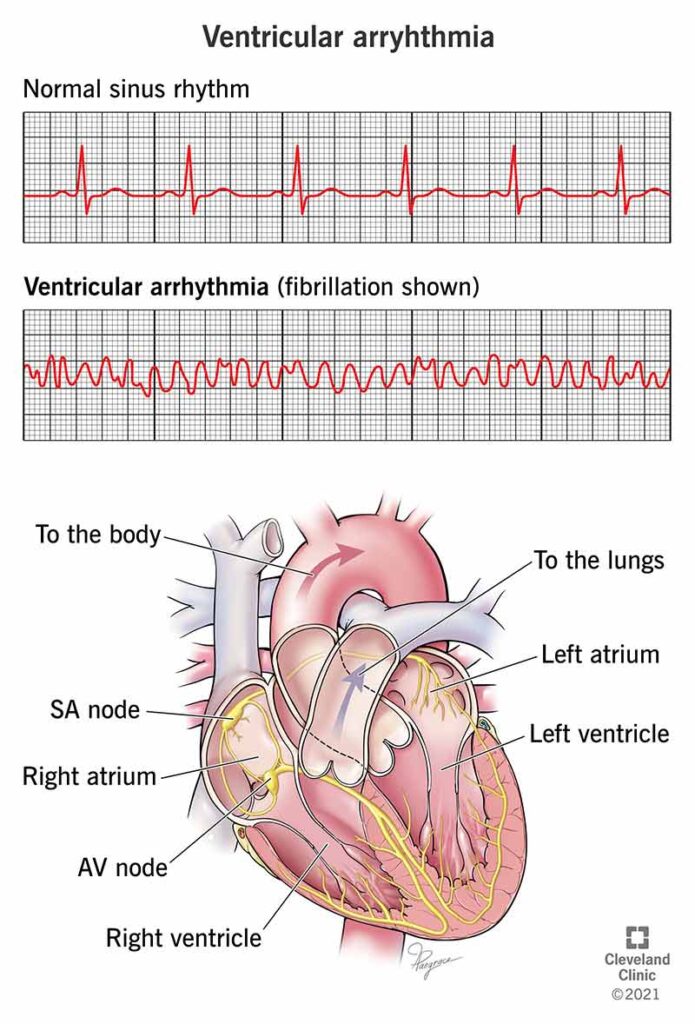
Electrocardiography (ECG)
- Wide QRS complexes (>120 ms)
- AV dissociation
- Fusion and capture beats
- Monomorphic VT shows consistent QRS morphology, whereas polymorphic exhibits variability.
Electrophysiological Study (EPS)
Used to localize the arrhythmogenic focus and guide ablation strategies, particularly in recurrent or idiopathic VT.
Imaging
- Echocardiography: Assesses structural anomalies.
- Cardiac MRI: Ideal for tissue characterization, especially fibrosis and scar.
- Coronary angiography: Evaluates ischemic causes when clinically indicated.
Management of Ventricular Tachycardia
Acute Management
- Hemodynamically unstable VT: Immediate synchronized cardioversion.
- Stable VT: Pharmacologic therapy using agents such as amiodarone or procainamide.
Advanced Life Support Measures
- High-energy defibrillation for pulseless VT
- ACLS algorithm adherence for cardiac arrest scenarios
Long-Term Management Strategies
Antiarrhythmic Drug Therapy
- Amiodarone: First-line agent in structural heart disease.
- Sotalol, Mexiletine, Lidocaine: Select indications based on etiology and comorbidities.
Catheter Ablation
Indicated in drug-refractory cases or patients with frequent ICD shocks. Success rates are higher in monomorphic VT.
Implantable Cardioverter-Defibrillator (ICD)
Gold standard in secondary prevention post-cardiac arrest or sustained VT. Also recommended in select primary prevention cohorts with reduced ejection fraction.
Special Considerations
Idiopathic Ventricular Tachycardia
Occurs in structurally normal hearts, often originating from the right ventricular outflow tract (RVOT). Prognosis is favorable and catheter ablation is frequently curative.
VT in Structural Heart Disease
High risk of recurrence and mortality. Requires comprehensive care involving ICDs, optimized heart failure therapy, and lifestyle adjustments.
Exercise-Induced VT
Requires evaluation for underlying channelopathies and may necessitate sports restriction or beta-blocker therapy.
Prognosis and Risk of Sudden Cardiac Death
VT significantly elevates the risk of sudden cardiac death (SCD), particularly in the context of left ventricular dysfunction. Risk stratification using ejection fraction, presence of fibrosis, and family history is essential to guide preventive interventions.
Prevention Strategies
- Optimize management of coronary artery disease and heart failure
- Regular ECG monitoring in high-risk populations
- Avoid QT-prolonging drugs
- Correct electrolyte imbalances proactively
- Genetic counseling and screening in inherited arrhythmia syndromes
Ventricular tachycardia is a complex arrhythmia with a wide range of etiologies and clinical implications. Prompt diagnosis, risk stratification, and tailored treatment strategies—ranging from pharmacologic therapy to ablation and ICD implantation—are vital for improving outcomes and preventing sudden cardiac death. A multidisciplinary approach remains the cornerstone of effective VT management.

