Ventricular premature beats (VPBs), also referred to as premature ventricular contractions (PVCs), are early depolarizations originating in the ventricles. They disrupt the normal rhythm of the heart by causing an extra, abnormal beat before the regular heartbeat resumes. While often benign, frequent VPBs may signify underlying cardiac pathology and can predispose to more serious arrhythmias in certain individuals.
Pathophysiology of Ventricular Premature Beats
VPBs originate from ectopic foci within the ventricular myocardium. Unlike normal beats initiated by the sinoatrial node, VPBs arise independently and interrupt the normal sinus rhythm. They do not allow sufficient time for ventricular filling and often result in a compensatory pause.
Causes of Ventricular Premature Beats
1. Physiological Causes
- Caffeine or nicotine consumption
- Emotional stress or anxiety
- Exercise-induced adrenergic surges
- Fatigue or lack of sleep
2. Pharmacologic Triggers
- Sympathomimetics (e.g., decongestants, amphetamines)
- Digitalis toxicity
- Antiarrhythmic drugs (proarrhythmic effect)
3. Electrolyte Imbalances
- Hypokalemia
- Hypomagnesemia
- Hypercalcemia
4. Structural Heart Disease
- Ischemic heart disease
- Cardiomyopathies
- Heart failure
- Valvular heart disorders
5. Idiopathic
- VPBs with no identifiable structural or metabolic abnormality
- Frequently arise from the right ventricular outflow tract (RVOT)
Clinical Features and Symptoms
VPBs may be asymptomatic and discovered incidentally during routine electrocardiography. When symptoms occur, they often include:
- Palpitations or fluttering sensation
- “Skipped” or “extra” heartbeats
- Chest discomfort
- Lightheadedness or fatigue
- Rarely, presyncope or syncope (in high burden or malignant forms)
The severity of symptoms is often disproportionate to the frequency of VPBs and more related to patient sensitivity.
Diagnostic Evaluation
1. Electrocardiogram (ECG)
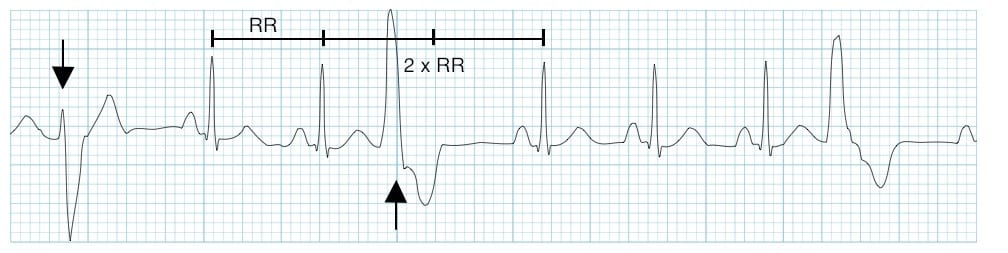
- Signature appearance: Wide QRS complex (>120 ms), not preceded by a P wave, followed by a compensatory pause
- Morphology:
- Monomorphic: consistent shape and origin
- Polymorphic: varying shapes indicating multiple foci
2. Holter Monitoring / Ambulatory ECG
- Records heart rhythm over 24 to 48 hours
- Quantifies VPB burden and correlates with symptoms
3. Exercise Stress Test
- Determines whether VPBs are suppressed or exacerbated during physical exertion
- Helps in distinguishing benign from ischemia-related VPBs
4. Echocardiography
- Evaluates structural abnormalities, ejection fraction, wall motion irregularities
5. Cardiac MRI (if indicated)
- Detects myocardial fibrosis or scar tissue
- Useful in evaluating arrhythmogenic right ventricular cardiomyopathy (ARVC)
Classification of VPBs
Based on Frequency:
- Isolated VPBs: Occur singly and sporadically
- Frequent VPBs: More than 30 per hour or >10% of total beats
- Bigeminy: Every alternate beat is a VPB
- Trigeminy: Every third beat is a VPB
- Couplets/Triplets: Two or three VPBs in succession
Based on Clinical Risk:
- Benign VPBs: No structural heart disease, normal ejection fraction
- Potentially Malignant VPBs: Associated with structural abnormalities
- Malignant VPBs: Trigger ventricular tachycardia or fibrillation
Management of Ventricular Premature Beats
1. Observation and Reassurance
- In asymptomatic individuals without structural heart disease, no treatment is required
- Lifestyle modifications such as reducing caffeine, alcohol, and stress are often sufficient
2. Pharmacologic Treatment
- Beta-blockers: First-line therapy in symptomatic patients or those with high VPB burden
- Calcium channel blockers: Alternatives in beta-blocker intolerance
- Antiarrhythmic drugs (e.g., flecainide, propafenone): Reserved for refractory cases, used with caution due to proarrhythmic potential
3. Catheter Ablation
- Highly effective for symptomatic monomorphic VPBs, particularly those arising from:
- Right ventricular outflow tract (RVOT)
- Left posterior fascicle
- Papillary muscles
- Considered when VPBs are >10–20% of total beats and linked to LV dysfunction
4. Treatment of Underlying Conditions
- Revascularization in ischemic heart disease
- Optimization of heart failure therapy
- Correction of electrolyte imbalances
Prognosis and Complications
In structurally normal hearts, VPBs typically have an excellent prognosis. However, frequent VPBs (>10% of total beats) may lead to:
- PVC-induced cardiomyopathy
- Ventricular tachycardia
- Sudden cardiac death (rare, in the presence of structural or electrical heart disease)
Timely diagnosis and tailored treatment can prevent these adverse outcomes and significantly improve quality of life.
Preventive Strategies
- Avoid known triggers (stimulants, stress, lack of sleep)
- Monitor and treat electrolyte disturbances
- Regular cardiac evaluations in high-risk individuals
- Early ablation in appropriate patients to prevent PVC-induced cardiomyopathy
Ventricular premature beats are common and often benign, but their evaluation should be comprehensive to exclude serious pathology. Accurate diagnosis through ECG and imaging, combined with individualized therapy—from reassurance to catheter ablation—ensures optimal outcomes. Early recognition and appropriate management are essential in preventing progression to more serious ventricular arrhythmias and preserving cardiac function.