Ventricular arrhythmias are potentially life-threatening cardiac rhythm disturbances originating from the ventricles. They range from benign premature ventricular complexes (PVCs) to lethal ventricular fibrillation (VF). These arrhythmias disrupt the heart’s ability to pump effectively, often resulting in hemodynamic instability, syncope, or sudden cardiac death (SCD).
Pathophysiology of Ventricular Arrhythmias
Abnormal ventricular rhythms are caused by one or more of the following electrophysiological mechanisms:
- Re-entry circuits
- Triggered activity
- Enhanced automaticity
Each mechanism alters the normal conduction pathway, leading to asynchronous contraction and impaired cardiac output.
Common Types of Ventricular Arrhythmias
1. Premature Ventricular Complexes (PVCs)
- Early beats originating from the ventricles
- Common in healthy individuals and patients with structural heart disease
- Usually benign unless frequent or multifocal
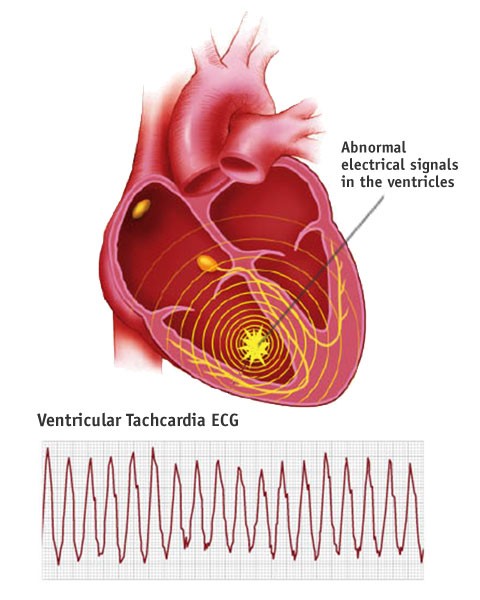
2. Ventricular Tachycardia (VT)
- Defined as three or more consecutive PVCs at a rate >100 bpm
- Can be:
- Sustained VT: lasts >30 seconds or requires intervention
- Nonsustained VT: self-terminating within 30 seconds
- Monomorphic VT: consistent QRS morphology
- Polymorphic VT: varying QRS shapes; includes torsades de pointes
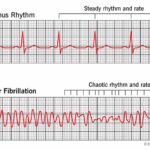
3. Ventricular Fibrillation (VF)
- Chaotic, disorganized ventricular activity
- No effective cardiac output
- Medical emergency requiring immediate defibrillation
Causes and Risk Factors
Ventricular arrhythmias are associated with multiple underlying conditions:
Structural Heart Disease
- Ischemic cardiomyopathy
- Myocardial infarction (scar-related re-entry)
- Dilated or hypertrophic cardiomyopathy
Genetic Syndromes
- Long QT Syndrome (LQTS)
- Brugada Syndrome
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
- Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
Other Risk Factors
- Electrolyte imbalances (hypokalemia, hypomagnesemia)
- Drug toxicity (digoxin, antiarrhythmics, QT-prolonging drugs)
- Heart failure and reduced ejection fraction
- Illicit drugs (e.g., cocaine, amphetamines)
Clinical Presentation
Symptoms may vary based on the type and severity of the arrhythmia:
- Palpitations
- Dizziness or lightheadedness
- Syncope
- Chest pain
- Dyspnea
- Sudden cardiac arrest (in VF or sustained VT)
Diagnostic Evaluation
Electrocardiogram (ECG)
- Primary tool for detecting and classifying ventricular arrhythmias
- VT shows wide-complex QRS with AV dissociation
Holter Monitoring & Ambulatory ECG
- Useful for detecting intermittent or asymptomatic episodes
Electrophysiological (EP) Study
- Invasive assessment to localize arrhythmogenic focus
- Guides ablation therapy
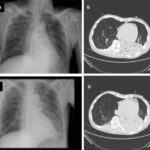
Cardiac Imaging
- Echocardiogram: evaluates structural heart disease
- Cardiac MRI: identifies fibrosis and ARVC
- Coronary angiography: assesses ischemic etiology
Management and Treatment Options
Acute Management
- Stable VT: IV antiarrhythmics (amiodarone, lidocaine)
- Unstable VT or VF: Immediate defibrillation and ACLS protocol
- Torsades de pointes: Magnesium sulfate and pacing
Chronic Management
1. Pharmacological Therapy
- Beta-blockers: first-line in many patients
- Amiodarone or sotalol for recurrent VT
- Avoid proarrhythmic drugs in patients with structural heart disease
2. Implantable Cardioverter-Defibrillator (ICD)
- Gold standard for secondary prevention post-cardiac arrest
- Indicated in:
- EF ≤35% and NYHA II/III
- Survivors of sustained VT/VF
- Inherited channelopathies with high risk of SCD
3. Catheter Ablation
- Effective in monomorphic VT due to scar-related re-entry
- Considered in:
- Refractory VT despite medical therapy
- Intolerable antiarrhythmic drug side effects
Prevention and Risk Stratification
Sudden Cardiac Death (SCD) Prevention
- Risk assessment via LVEF, Holter findings, family history
- Genetic testing in inherited arrhythmia syndromes
- Lifestyle modifications (e.g., avoiding QT-prolonging agents)
Secondary Prevention
- ICD placement after cardiac arrest or sustained VT
- Optimization of heart failure therapy
- Close monitoring in patients with high arrhythmic burden
Prognosis
Prognosis varies based on etiology, arrhythmia type, and treatment adequacy. Patients with structurally normal hearts and benign PVCs have excellent outcomes. Conversely, those with structural heart disease and sustained VT or VF are at higher risk for SCD.
Predictors of adverse outcomes include:
- Left ventricular dysfunction
- Frequent PVCs or nonsustained VT
- History of syncope or cardiac arrest
- Lack of ICD protection in high-risk individuals
Ventricular arrhythmias represent a spectrum of ventricular-originated rhythm disturbances that demand a precise, individualized approach. Prompt identification, risk stratification, and appropriate therapy—including ICD implantation, pharmacologic control, or ablation—are crucial in reducing morbidity and mortality. Preventive strategies and technological advancements in diagnostics and therapy continue to improve outcomes for patients at risk.