Vancomycin-resistant Enterococcus faecium (VRE) is an opportunistic, multidrug-resistant pathogen and a major cause of nosocomial infections. It poses a significant challenge in healthcare settings due to its ability to colonize, persist in the environment, and resist first-line antimicrobial agents. Infections range from asymptomatic colonization to life-threatening conditions such as bacteremia, urinary tract infections, endocarditis, and intra-abdominal infections.
Molecular Basis of Vancomycin Resistance in E. faecium
Genetic Determinants
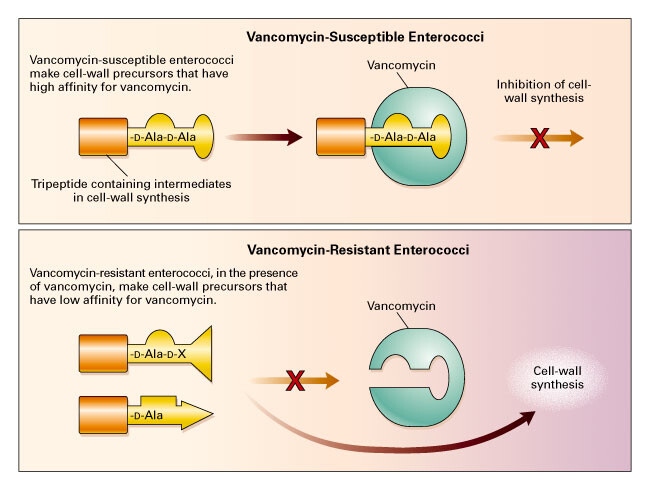
Vancomycin resistance in E. faecium is primarily mediated by the vanA and vanB gene clusters, which alter the terminal D-Ala-D-Ala dipeptide of the peptidoglycan precursor to D-Ala-D-Lac. This modification reduces vancomycin’s binding affinity by a factor of 1000, rendering the antibiotic ineffective.
Epidemiology and Transmission Dynamics
VRE has a well-documented capacity for clonal dissemination in hospitals and long-term care facilities. Its epidemiology is influenced by geographic region, antibiotic stewardship practices, and infection control measures.
- Reservoirs: Human gastrointestinal tract, contaminated surfaces, and medical equipment.
- Modes of Transmission: Direct contact via hands of healthcare personnel, or indirectly via the hospital environment.
Clinical Manifestations of VRE Infections
Common Infections
- Bloodstream Infections
Frequently associated with central venous catheters, these are the most severe form and carry high mortality rates. - Urinary Tract Infections (UTIs)
Often asymptomatic but may progress to complicated infections, particularly in catheterized patients. - Wound and Surgical Site Infections
Typically occur in post-operative or immunocompromised patients. - Endocarditis
Rare but highly lethal, often requiring combination therapy and prolonged treatment.
Risk Factors
- Recent antibiotic exposure (particularly vancomycin or cephalosporins)
- Immunosuppression
- Indwelling medical devices
- Extended hospital or ICU stays
Diagnostic Approaches to Identify VRE
Microbiological Techniques
- Culture-Based Detection: Blood, urine, or wound swabs cultured on selective media containing vancomycin.
- Identification: Use of MALDI-TOF MS or biochemical testing to confirm E. faecium species.
- Antibiotic Susceptibility Testing (AST): Automated or manual methods confirm resistance profiles.
Molecular Diagnostics
- PCR Testing: Detects vanA and vanB genes rapidly and with high specificity.
- Whole Genome Sequencing (WGS): Employed for outbreak investigation and resistance gene tracking.
Management and Treatment of VRE Infections
First-Line Antimicrobial Agents
| Antibiotic | Mechanism | Clinical Considerations |
|---|---|---|
| Linezolid | Protein synthesis inhibition | Oral and IV; risk of thrombocytopenia, serotonin syndrome |
| Daptomycin | Cell membrane depolarization | Bactericidal; monitor for myopathy; not for pneumonia |
| Tigecycline | 30S ribosomal inhibition | Not suitable for bloodstream infections |
| Quinupristin/Dalfopristin | Ribosomal inhibition | Effective against E. faecium only; limited by side effects |
| Oritavancin/Dalbavancin | Cell wall inhibition | Extended half-life; emerging therapies |
Combination Therapy
In severe or persistent infections, especially endocarditis, combination regimens involving linezolid or daptomycin with other agents such as ampicillin or rifampin are considered to enhance bactericidal activity.
Infection Control and Hospital-Based Interventions
Key Measures
- Contact Precautions: Gown and glove use, patient isolation, dedicated medical equipment.
- Active Surveillance Cultures: Regular screening in high-risk wards like ICUs or oncology.
- Environmental Cleaning: Daily disinfection of high-touch surfaces with agents effective against gram-positive cocci.
- Hand Hygiene Compliance: Critical component in breaking the chain of transmission.
Antimicrobial Stewardship
- Reduction in unnecessary vancomycin and broad-spectrum antibiotic use.
- Implementation of formulary restrictions and real-time prescription audits.
Global Trends and Resistance Surveillance
Organizations such as the Centers for Disease Control and Prevention (CDC) and the European Centre for Disease Prevention and Control (ECDC) actively monitor VRE prevalence. Regional variations in resistance rates are tied to differing antibiotic practices and infection control policies.
- North America: High rates in tertiary care hospitals.
- Europe: Eastern regions report increasing resistance.
- Asia: Variable, but emerging resistance due to unregulated antibiotic use.
Emerging Therapies and Future Prospects
- Novel Antibiotics: Development of next-generation oxazolidinones, lipoglycopeptides, and bacteriophage therapies.
- CRISPR-Based Gene Editing: Experimental approaches to selectively eliminate resistance genes.
- Microbiota Restoration: Use of fecal microbiota transplantation (FMT) to eradicate gastrointestinal colonization.
Vancomycin-resistant Enterococcus faecium infection remains a critical clinical and public health issue. Its capacity for resistance development, environmental persistence, and patient-to-patient transmission necessitates a multifaceted approach incorporating prompt diagnosis, optimized antimicrobial therapy, and rigorous infection prevention protocols. Ongoing research into novel therapeutics and diagnostics holds promise in mitigating the burden of VRE in healthcare systems worldwide.