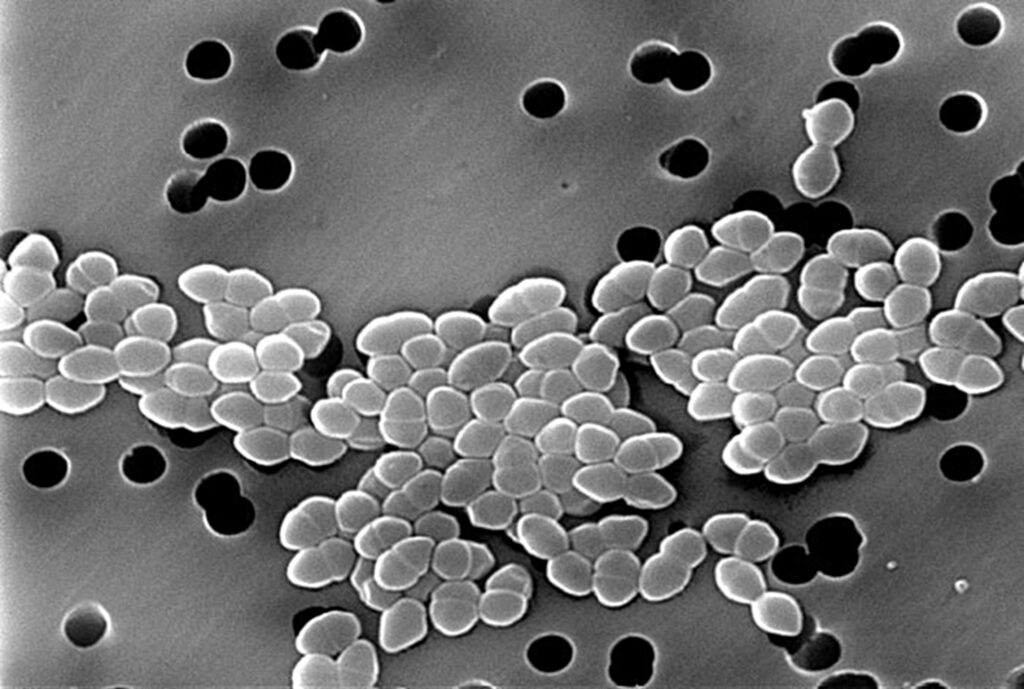
Vancomycin-resistant Enterococcus faecium (VRE) represents a formidable nosocomial pathogen, responsible for a growing number of bloodstream infections worldwide. These infections predominantly affect immunocompromised patients, individuals with prolonged hospital stays, and those exposed to broad-spectrum antibiotic therapy. Due to limited therapeutic options, high transmission potential, and increased morbidity and mortality, VRE bacteremia has emerged as a major public health threat in healthcare settings.
Pathogenesis of VRE Bacteremia
Mechanisms of Resistance
The resistance to vancomycin in E. faecium is largely mediated by the vanA and vanB gene clusters, which alter the target site of vancomycin from D-Ala-D-Ala to D-Ala-D-Lac, significantly reducing the drug’s binding affinity.
Host and Environmental Factors
- Immunosuppression: Cancer patients, transplant recipients, and ICU patients are particularly vulnerable.
- Antibiotic Overuse: Use of cephalosporins and vancomycin disrupts normal flora and promotes VRE colonization.
- Biofilm Formation: Enhances survival on medical devices and resistance to host immune response.
Clinical Presentation of VRE Bloodstream Infections
Symptoms and Signs
Patients with VRE bacteremia often present with:
- High-grade fever
- Hypotension
- Chills and rigors
- Organ dysfunction in severe sepsis
Infections may originate from central venous catheters, surgical wounds, urinary tract infections, or the gastrointestinal tract.
Diagnostic Approaches
Laboratory Identification
- Blood Cultures: Growth in routine aerobic blood cultures within 24–72 hours.
- MALDI-TOF MS: Rapid species-level identification of Enterococcus faecium.
- Antimicrobial Susceptibility Testing (AST): Confirms vancomycin resistance via broth microdilution or automated systems.
Molecular Testing
- PCR Assays: Detect vanA/vanB genes with high sensitivity and specificity.
- Whole Genome Sequencing (WGS): Provides insights into resistance mechanisms, epidemiology, and clonal spread.
Therapeutic Management of VRE Bacteremia
Limited Antimicrobial Options
Due to intrinsic resistance and vancomycin non-susceptibility, treatment regimens are limited. Empirical therapy should consider local susceptibility patterns.
| Antimicrobial Agent | Mechanism | Use Consideration |
|---|---|---|
| Linezolid | Protein synthesis inhibitor (50S ribosome) | First-line; oral and IV; bone marrow suppression risk |
| Daptomycin | Membrane depolarization | Bactericidal; not for pneumonia; monitor CPK |
| Tigecycline | Glycylcycline; 30S inhibitor | Limited bacteremia data; high tissue distribution |
| Quinupristin/Dalfopristin | Streptogramin B and A combo | Limited by adverse effects; inactive against E. faecalis |
| Oritavancin/Dalbavancin | Lipoglycopeptides | Under investigation; long half-life |
Infection Control and Prevention
Surveillance and Screening
- Active surveillance in high-risk wards (e.g., ICU, oncology)
- Rectal swabs for VRE colonization detection
Contact Precautions
- Isolation of colonized/infected patients
- Use of gowns and gloves
- Dedicated equipment to prevent cross-contamination
Environmental Decontamination
- Rigorous cleaning with sporicidal disinfectants
- Emphasis on high-touch surfaces
Antimicrobial Stewardship
- Restriction of vancomycin and cephalosporin use
- Promotion of narrow-spectrum, targeted therapy
Epidemiology and Global Burden
- North America: High prevalence in tertiary care hospitals
- Europe: Variable incidence; increasing trend noted
- Asia-Pacific: Rapidly emerging resistance due to unregulated antibiotic use
- WHO Priority Pathogen List: VRE is listed among high-priority antibiotic-resistant pathogens.
Prognosis and Mortality
- Mortality rates range from 25% to 50%, particularly in immunocompromised or septic patients.
- Delay in initiating effective therapy is a critical factor influencing outcomes.
- VRE bacteremia often prolongs hospital stay and increases healthcare costs substantially.
Future Directions in VRE Research
- Development of Novel Agents: New lipoglycopeptides, oxazolidinones, and bacteriophage therapy.
- Vaccination Strategies: Targeting enterococcal surface proteins.
- Microbiota Modulation: Fecal microbiota transplantation (FMT) to eradicate colonization.
Vancomycin-resistant Enterococcus faecium bacteremia presents a significant challenge in modern healthcare due to its resistance profile, limited treatment options, and high mortality. Prompt diagnosis, targeted therapy, and stringent infection control are crucial for managing this formidable pathogen. Ongoing research and antibiotic stewardship are imperative to curb the spread and impact of VRE in clinical settings.