Vaginal hysterectomy is a minimally invasive procedure preferred for treating benign gynecological conditions such as fibroids, uterine prolapse, and abnormal bleeding. Despite its advantages—reduced recovery time, minimal scarring, and shorter hospital stays—this surgery carries a risk of post-operative infections, including surgical site infections (SSIs), vaginal cuff cellulitis, and pelvic abscesses. Implementing a thorough, protocol-driven infection prevention strategy is critical to ensuring patient safety and promoting rapid recovery.
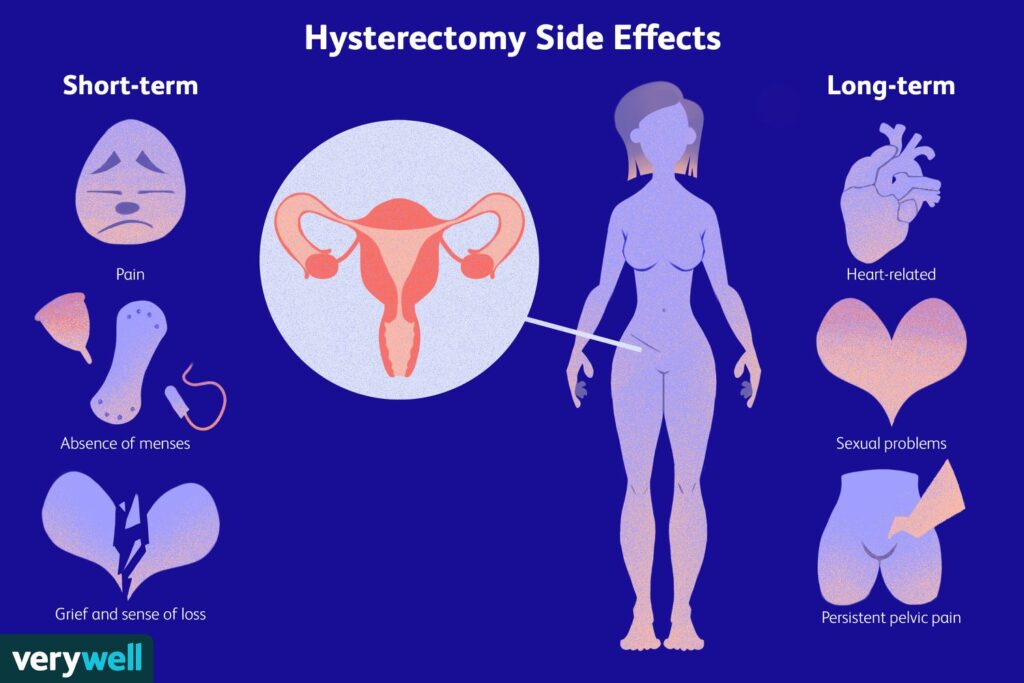
Common Types of Infections After Vaginal Hysterectomy
- Vaginal Cuff Cellulitis
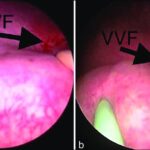
Inflammation at the closure site of the vaginal cuff, often caused by ascending bacteria. - Pelvic Abscess
Localized collection of pus in the pelvic cavity, frequently polymicrobial and anaerobic in nature. - Urinary Tract Infections (UTIs)
Often associated with catheterization during surgery. - Wound Infection (in rare laparoscopic-assisted cases)
Especially in patients undergoing combined procedures. - Sepsis
A rare but serious systemic response to an uncontrolled local infection.
Risk Factors That Elevate Infection Rates
Several modifiable and non-modifiable factors contribute to postoperative infection risks:
| Category | Risk Factor |
|---|---|
| Patient-related | Obesity, diabetes, smoking, anemia |
| Surgical | Prolonged duration, contamination |
| Environmental | Non-sterile instruments, poor airflow |
| Post-operative | Poor wound care, early intercourse |
| Microbiological | Vaginal flora imbalance, resistant organisms |
Preoperative Protocols for Infection Prevention
1. Pre-Surgical Screening and Optimization
- Control of blood glucose levels in diabetic patients.
- Cessation of smoking at least 2 weeks prior to surgery.
- Treatment of existing vaginal infections (e.g., bacterial vaginosis, candidiasis).
- Anemia correction to support healing.
2. Antibiotic Prophylaxis
Administer a single dose of prophylactic antibiotics—typically cefazolin or a combination of cefazolin and metronidazole—30 to 60 minutes before incision.
3. Vaginal Preparation
Use povidone-iodine or chlorhexidine vaginal scrub immediately before surgery to reduce bacterial load.
Intraoperative Measures to Minimize Infection
1. Maintaining Aseptic Technique
Strict adherence to sterile protocols throughout the surgical team is non-negotiable.
2. Minimizing Blood Loss and Tissue Trauma
Reducing trauma minimizes necrosis, which could act as a nidus for bacterial colonization.
3. Vaginal Cuff Closure Technique
Secure, tension-free sutures using absorbable material lowers the risk of cuff dehiscence and infection.
Postoperative Care: Infection Surveillance and Prevention
1. Wound and Cuff Monitoring
- Daily evaluation of discharge volume, odor, and color
- Speculum exams during follow-up to inspect the vaginal cuff
2. Catheter and UTI Prevention
- Remove Foley catheters within 24 hours
- Encourage early ambulation and hydration
3. Antibiotic Stewardship
Avoid prolonged or unnecessary postoperative antibiotics unless clinical signs of infection appear.
4. Patient Education
- Hygiene Practices: No douching or tampons
- Activity Restrictions: Avoid heavy lifting and sexual activity for at least 6 weeks
- Symptom Reporting: Immediate medical attention for fever, unusual discharge, or severe pain
Advanced Prevention Tactics for High-Risk Patients
Diabetic Patients
- Continuous blood sugar monitoring in the perioperative period
- Insulin adjustments as needed
Immunocompromised Patients
- May require extended antimicrobial coverage or inpatient observation
Obese Patients
- Preoperative weight management program
- Modified surgical positioning to reduce operative time and improve visualization
Frequently Asked Questions:
What is the most common infection after vaginal hysterectomy?
Vaginal cuff cellulitis remains the most frequently encountered infection, often presenting with fever and foul-smelling discharge.
How soon do infections develop post-hysterectomy?
Infections typically arise within 3 to 7 days post-surgery but can develop later depending on individual healing and hygiene.
Can vaginal infection be prevented completely?
While absolute prevention is not always possible, the risk can be significantly reduced through strict adherence to protocols.
When should I contact my doctor after surgery?
If you notice persistent fever, abdominal pain, foul discharge, or chills, contact your provider immediately.
Do I need antibiotics after hysterectomy?
Only preoperative prophylaxis is routinely recommended unless an infection develops postoperatively.
Effective vaginal hysterectomy infection prevention is a collaborative effort involving careful preoperative preparation, intraoperative discipline, and postoperative vigilance. By integrating evidence-based protocols, personalized risk management, and consistent patient education, we can significantly reduce infection rates and improve surgical outcomes. Preventing infection is not a single step but a continuum of care that demands attention at every stage of the patient journey.