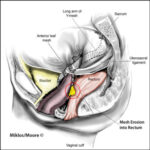
Vaginal cuff surgery is performed during total hysterectomy procedures to close the top of the vaginal canal after the removal of the uterus and cervix. Although typically uneventful, this surgical site is susceptible to post-operative infections, especially by anaerobic organisms such as Peptococcus. These infections can complicate recovery, delay wound healing, and, if untreated, lead to serious intra-abdominal or pelvic complications.
Understanding Peptococcus and Its Role in Post-Operative Infections
Peptococcus is a genus of anaerobic gram-positive cocci commonly found in the normal flora of the oral cavity, gastrointestinal tract, and vagina. Under surgical stress or tissue damage, this normally benign organism can become opportunistic, leading to infections within the closed environment of the vaginal cuff post-hysterectomy. These infections often occur polymicrobially, in concert with other anaerobes and facultative bacteria.
Mechanism of Peptococcus Infection Post Vaginal Cuff Surgery
The pathogenesis involves the translocation or introduction of Peptococcus into the surgical wound, where the anaerobic environment facilitates its rapid proliferation. Risk factors enhancing this colonization include poor aseptic technique, retained blood or necrotic tissue, immunosuppression, and disruption of normal vaginal flora through antibiotics or douching.
Clinical Presentation of Post-Op Peptococcus Infection
Symptoms may appear within 3–14 days following surgery, though delayed presentations are possible. Hallmark features include:
- Persistent pelvic or lower abdominal pain
- Malodorous vaginal discharge with a yellowish or brownish tint
- Low-grade or intermittent fever
- Tenderness on vaginal or abdominal exam
- Delayed wound healing or suture line separation
- Systemic signs such as fatigue, chills, or night sweats in advanced infections
Because Peptococcus thrives in low-oxygen environments, these infections are often deep-seated and may present subtly compared to more aggressive aerobic infections.
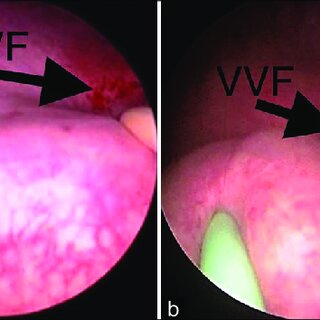
Diagnostic Approach for Vaginal Cuff Peptococcus Infection
Clinical Evaluation
A thorough physical and pelvic examination remains foundational. Findings of purulence at the cuff or foul odor warrant further investigation.
Laboratory and Microbiological Tests
- CBC with Differential: Leukocytosis with left shift
- CRP and ESR: Elevated in ongoing inflammation
- Gram stain and anaerobic culture of vaginal discharge or aspirate: Identification of Peptococcus
- Blood cultures: If systemic symptoms or fever is present
- Anaerobic sensitivity testing: Crucial for tailoring antibiotic therapy
Imaging Modalities
- Transvaginal Ultrasound: Detects fluid collection or abscess
- CT Pelvis with contrast: Evaluates extent of soft tissue involvement and deep pelvic infection
- MRI Pelvis (if needed): Provides high-resolution soft tissue detail
Treatment Strategies for Peptococcus Post-Op Infection
Antibiotic Therapy
Empiric treatment must cover anaerobic flora, with specific coverage for Peptococcus. Upon culture confirmation, targeted therapy should be initiated. Options include:
- Clindamycin 600–900 mg IV q8h or oral equivalent
- Metronidazole 500 mg IV or PO q8–12h
- Piperacillin-tazobactam for broad-spectrum anaerobic coverage
- Penicillin G in sensitive isolates
- Moxifloxacin as an oral alternative in mild infections
Therapy typically continues for 10–14 days, longer if an abscess or dehiscence is involved.
Surgical Management
Infection control may necessitate minor or major interventions:
- Irrigation and debridement of vaginal cuff under sterile conditions
- Incision and drainage of pelvic abscesses
- Laparoscopic lavage or drainage if peritoneal spread occurs
- Resuturing or reinforcement if dehiscence is identified
Close postoperative monitoring is essential to evaluate response and detect complications.
Complications Associated with Untreated Peptococcus Infections
- Vaginal cuff dehiscence
- Pelvic abscess formation
- Sepsis and multi-organ failure
- Pelvic adhesions and chronic pain
- Extended hospitalization and recovery delays
Early recognition and management are crucial to avoid escalation and preserve patient quality of life.
Preventive Measures Against Post-Surgical Peptococcus Infection
Preoperative Protocols
- Vaginal antiseptic cleansing
- Prophylactic antibiotics within 60 minutes before incision
- Glycemic control in diabetic patients
- Correction of anemia or nutritional deficiencies pre-surgery
Intraoperative Best Practices
- Sterile technique and minimal use of electrocautery
- Ensuring hemostasis to prevent hematoma formation
- Adequate closure with absorbable sutures
- Copious irrigation with saline or antimicrobial solution
Postoperative Care Guidelines
- Avoidance of sexual activity for 6–8 weeks
- Monitoring for fever or abnormal discharge
- Educating patients on signs of infection
- Regular wound checks during follow-up visits
Recovery Outlook and Long-Term Prognosis
With prompt diagnosis and appropriate antibiotic therapy, most patients recover without permanent sequelae. Severe cases involving abscesses or systemic spread may necessitate prolonged treatment and follow-up. Full recovery can be expected within 4–8 weeks, though residual fatigue or pelvic discomfort may persist temporarily.
Patients are advised to maintain good hygiene, follow postoperative instructions diligently, and report new symptoms without delay.
Frequently Asked Questions
What makes Peptococcus infections difficult to detect?
As an anaerobe, Peptococcus causes subtle or insidious symptoms, often mimicking post-surgical fatigue or minor healing disturbances.
Can Peptococcus cause infections without fever?
Yes. Many anaerobic infections, including those from Peptococcus, may occur without high fever but present with foul discharge and localized pain.
Is this infection preventable?
Yes. Prevention includes proper surgical technique, prophylactic antibiotics, and diligent postoperative care.
Can Peptococcus lead to vaginal cuff dehiscence?
Yes. Chronic infection can weaken sutures, impair tissue healing, and cause dehiscence.
What should I avoid after vaginal cuff surgery?
Refrain from sexual intercourse, douching, swimming, and heavy lifting for at least six weeks unless directed otherwise by your provider.
Post-operative Peptococcus infection following vaginal cuff surgery, though uncommon, represents a clinically significant complication that requires a high index of suspicion and timely intervention. Accurate diagnosis, culture-guided antibiotic therapy, and preventive strategies ensure optimal outcomes and a return to health. We emphasize strict adherence to perioperative protocols and patient education to minimize risk and promote seamless recovery.