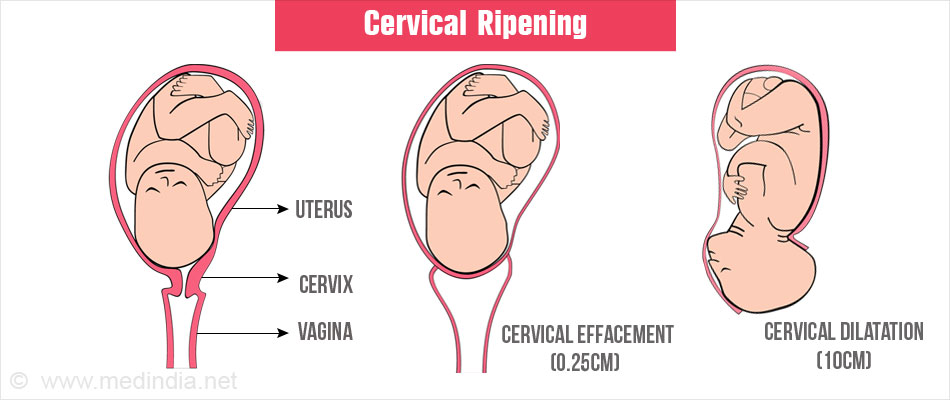
Cervical ripening is a critical step in preparing for labor and childbirth. It involves softening and dilating the cervix to enable the passage of the baby through the birth canal. This procedure is essential when labor does not begin naturally or when medical induction is necessary. In this guide, we explore the various aspects of cervical ripening, including its methods, indications, risks, and benefits.
Understanding Cervical Ripening
Cervical ripening refers to the physiological and medical processes that prepare the cervix for labor. The cervix, a cylindrical tissue connecting the uterus to the vagina, undergoes softening, thinning, and dilation during this process. These changes are influenced by hormonal shifts and, when necessary, medical interventions.
Why Is Cervical Ripening Necessary?
- Prolonged Pregnancy: When pregnancy extends beyond 41 weeks, cervical ripening may be required to initiate labor.
- Medical Conditions: Conditions such as preeclampsia, diabetes, or fetal growth restriction may necessitate labor induction.
- Non-progressive Labor: In some cases, the cervix does not dilate sufficiently despite uterine contractions, requiring intervention.
Methods of Cervical Ripening
Cervical ripening can be achieved through medical and mechanical techniques. Each method is selected based on the patient’s medical history, gestational age, and specific circumstances.
1. Pharmacological Methods
a. Prostaglandins
Prostaglandins are hormones that promote cervical softening and uterine contractions. They are administered in the form of vaginal gels, tablets, or suppositories.
- Common Types: Misoprostol and Dinoprostone
- Advantages: Effective for cervical dilation and initiating labor
- Considerations: Requires close monitoring for hyperstimulation of the uterus
b. Oxytocin
Although primarily used for labor induction, oxytocin can complement other cervical ripening methods to enhance effectiveness.
2. Mechanical Methods
a. Balloon Catheter
A balloon catheter, such as a Foley catheter, is inserted into the cervix and inflated to apply gentle pressure. This stimulates the release of natural prostaglandins and promotes cervical dilation.
- Advantages: Non-pharmacological, minimal systemic effects
- Considerations: May cause discomfort during insertion
b. Hygroscopic Dilators
Hygroscopic dilators, such as laminaria or synthetic alternatives, absorb moisture and expand, gradually dilating the cervix.
- Advantages: Slow and controlled dilation
- Considerations: May require multiple applications
3. Alternative Methods
a. Membrane Sweeping
A healthcare provider separates the amniotic sac from the uterine wall using a gloved finger during a vaginal exam. This action stimulates natural prostaglandin production.
- Advantages: Can initiate labor naturally
- Considerations: May cause discomfort or spotting
b. Herbal and Complementary Approaches
Some women consider herbal supplements or acupuncture for cervical ripening. However, these methods lack robust scientific validation and should be discussed with a healthcare provider.
Risks and Considerations
While cervical ripening is generally safe, it carries potential risks. These include:
- Uterine Hyperstimulation: Excessive contractions that may compromise oxygen supply to the baby
- Infection: Particularly with mechanical methods
- Discomfort or Pain: Common with mechanical interventions
- Failure to Progress: Cervical ripening may not always lead to successful labor induction, necessitating cesarean delivery
Benefits of Cervical Ripening
- Reduced Need for Cesarean Delivery: Successful ripening increases the likelihood of vaginal birth.
- Facilitates Labor Induction: Prepares the cervix for effective contractions
- Improved Maternal Outcomes: Minimizes risks associated with prolonged pregnancy or unplanned emergency interventions
Preparing for the Procedure
Before undergoing cervical ripening, your healthcare provider will:
- Assess Medical History: To determine the safest approach
- Perform a Physical Examination: Including a pelvic exam to evaluate cervical status using the Bishop Score
- Discuss Options: Explaining the risks, benefits, and expected outcomes
Recovery and Follow-Up
After the procedure, patients are monitored for signs of labor onset and potential complications. Hospitalization may be required depending on the method used and the progression of labor.