Vagal reflex bradycardia refers to a sudden, reflex-mediated reduction in heart rate caused by activation of the vagus nerve. This autonomic response, primarily parasympathetic in nature, is a protective mechanism that can become pathologic under certain stimuli. Understanding the underlying physiology and clinical relevance is vital for managing patients prone to syncope or bradyarrhythmias.
Physiology of the Vagus Nerve in Cardiac Regulation
The vagus nerve (cranial nerve X) plays a central role in parasympathetic modulation of the heart. It innervates the sinoatrial (SA) and atrioventricular (AV) nodes, influencing chronotropy and dromotropy. Activation of the vagus nerve releases acetylcholine, which binds to muscarinic receptors, resulting in:
- Decreased SA node firing rate
- Prolongation of AV node conduction
- Potential atrioventricular block in severe cases
This physiological effect ensures cardiovascular stability but can precipitate bradycardia when exaggerated.
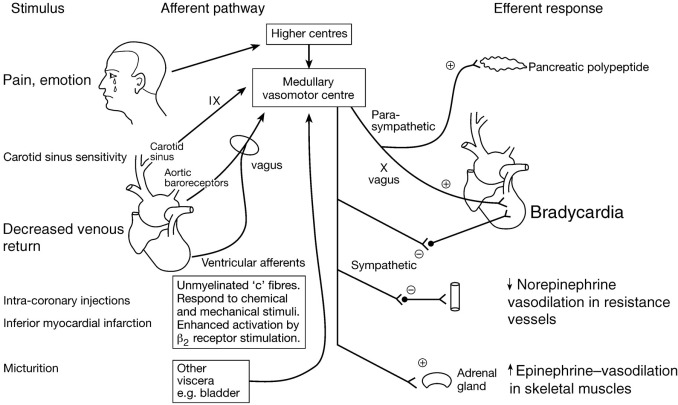
Reflex Pathways Involved in Vagal-Induced Bradycardia
Key Reflex Arcs
Several reflex mechanisms can trigger vagal bradycardia, including:
- Vasovagal Reflex (Neurocardiogenic Reflex): Often triggered by stress, pain, or prolonged standing.
- Oculocardiac Reflex: Occurs during ocular manipulation or surgery.
- Carotid Sinus Reflex: Stimulated by pressure on the carotid sinus (e.g., tight collars, head turning).
- Trigeminal-Cardiac Reflex: Initiated by stimulation of trigeminal nerve branches during craniofacial procedures.
Common Clinical Scenarios Associated with Vagal Reflex Bradycardia
Syncope and Presyncope
Vagal reflex bradycardia is a key contributor to reflex syncope, characterized by sudden cerebral hypoperfusion. Symptoms include dizziness, nausea, pallor, and transient loss of consciousness.
Intraoperative Bradycardia
Surgeons may encounter bradycardia during procedures involving the eyes, face, neck, or abdomen due to vagal stimulation. Prompt cessation of the triggering maneuver typically resolves the episode.
Carotid Sinus Hypersensitivity
Common in elderly individuals, this condition leads to exaggerated vagal response upon carotid baroreceptor stimulation, resulting in bradycardia or asystole.
Diagnostic Approaches
Electrocardiogram (ECG)
- Bradycardia: Defined as heart rate <60 bpm
- Sinus pause or AV block during reflex episodes
Tilt Table Testing
Used to provoke and analyze vasovagal responses, particularly in recurrent syncope cases.
Carotid Sinus Massage
Helps identify carotid sinus hypersensitivity, with ECG monitoring required to detect bradyarrhythmia.
Management of Vagal Reflex Bradycardia
Acute Treatment
- Trendelenburg position to increase venous return
- Atropine (0.5 mg IV) to inhibit parasympathetic activity
- Cessation of stimulus (e.g., stop ocular traction)
Chronic Management
- Education on trigger avoidance
- Volume expansion with increased salt/fluid intake
- Beta-blockers (in some paradoxical cases)
- Permanent pacemaker implantation for severe cardioinhibitory reflex syncope
Clinical Guidelines for Pacemaker Indication
| Condition | Indication |
|---|---|
| Recurrent syncope with documented asystole | Class I indication for pacing |
| Carotid sinus syndrome with pause >3 sec | Pacing considered |
| Neurocardiogenic syncope unresponsive to drugs | Consider dual-chamber pacemaker |
Prevention Strategies
- Avoid known triggers (heat, pain, emotional stress)
- Encourage slow positional changes to prevent orthostatic reflex
- Pre-operative vagolytic prophylaxis in high-risk surgeries
- Wear loose collars for patients with carotid sinus sensitivity
Prognosis and Outcomes
Most cases of vagal reflex bradycardia are benign and self-limiting. However, in severe or recurrent episodes, particularly those with trauma from syncope-related falls, clinical intervention significantly improves quality of life and reduces recurrence.
FAQs:
What triggers vagal reflex bradycardia?
Common triggers include pain, emotional distress, ocular pressure, carotid sinus stimulation, and gastrointestinal procedures.
How is it different from other bradycardias?
It is reflex-mediated and typically reversible upon removal of the stimulus, unlike intrinsic conduction system diseases.
Can vagal reflex bradycardia be dangerous?
While often benign, it may cause syncope or even cardiac arrest in extreme cases, especially in carotid sinus syndrome.
Is it treatable?
Yes, treatment options range from lifestyle changes and medication to pacemaker implantation in severe cases.
Should a patient with recurrent episodes see a specialist?
Yes, evaluation by a cardiologist or electrophysiologist is recommended for persistent or unexplained bradycardia.

