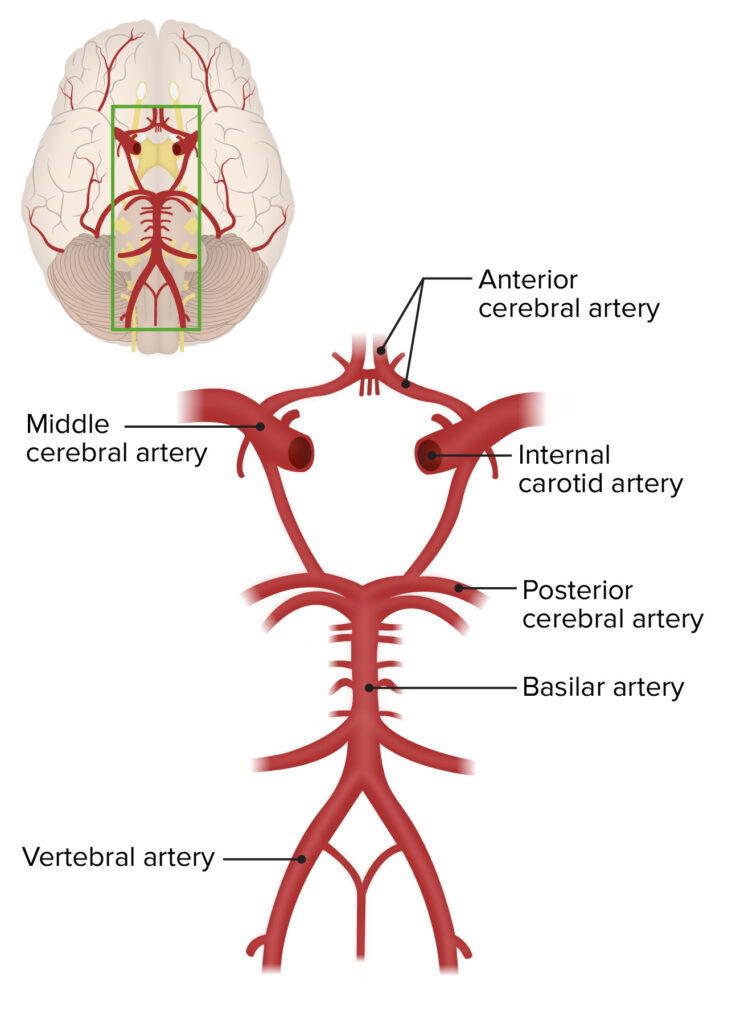
Cerebrovascular occlusion refers to the blockage of blood flow within the blood vessels of the brain. This condition can lead to severe complications, including ischemic strokes, as the brain tissue is deprived of essential oxygen and nutrients. Prompt recognition and management of cerebrovascular occlusion are critical to minimizing damage and improving outcomes.
Causes of Cerebrovascular Occlusion
1. Atherosclerosis
Atherosclerosis is a common cause, where fatty deposits build up along arterial walls, narrowing the lumen and restricting blood flow. Over time, these plaques may rupture, leading to thrombus formation and vascular occlusion.
2. Embolism
An embolus, often a blood clot or fatty deposit, may travel through the bloodstream and lodge in a cerebral artery, causing a sudden blockage. Common sources include:
- Atrial fibrillation
- Deep vein thrombosis (DVT)
- Fat embolism from bone fractures
3. Thrombosis
Localized clot formation within a cerebral vessel can obstruct blood flow. This is often associated with:
- Prolonged immobility
- Hypercoagulable states
- Certain cancers
4. Vasculitis
Inflammation of blood vessels, often due to autoimmune disorders, can lead to narrowed or blocked arteries.
5. Trauma and Dissection
Trauma-induced vascular dissection can restrict blood flow, especially in the carotid or vertebral arteries.
Recognizing Symptoms
The symptoms of cerebrovascular occlusion vary depending on the affected brain region. Common indicators include:
- Sudden weakness or numbness on one side of the body
- Facial drooping, especially on one side
- Difficulty speaking or understanding speech
- Loss of coordination or balance
- Severe headache with no known cause
- Vision changes, including loss of vision in one eye or double vision
Diagnosis of Cerebrovascular Occlusion
1. Clinical Assessment
Neurological examinations assess symptoms and determine the affected brain region. The National Institutes of Health Stroke Scale (NIHSS) is often employed.
2. Imaging Studies
- CT Scan: Quickly identifies ischemic or hemorrhagic strokes.
- MRI: Provides detailed images of brain tissue and detects early signs of ischemia.
- CT or MR Angiography: Visualizes blood vessels to pinpoint occlusions.
3. Laboratory Tests
Blood tests may identify risk factors such as high cholesterol, hypercoagulability, or underlying infections.
Treatment Options
1. Acute Management
Thrombolytic Therapy
Intravenous tissue plasminogen activator (tPA) is administered within 4.5 hours of symptom onset to dissolve clots and restore blood flow.
Endovascular Intervention
Mechanical thrombectomy involves the physical removal of clots via catheter-based techniques. This is particularly effective for large vessel occlusions.
2. Secondary Prevention
Antiplatelet Agents
Medications such as aspirin and clopidogrel reduce the risk of future clots.
Anticoagulation Therapy
For patients with conditions like atrial fibrillation, anticoagulants like warfarin or direct oral anticoagulants (DOACs) are prescribed.
Lifestyle Modifications
- Smoking cessation
- Dietary adjustments to lower cholesterol
- Regular physical activity
- Blood pressure control
Prognosis and Recovery
Outcomes depend on the severity of the occlusion, the speed of treatment, and the presence of comorbidities. Early rehabilitation, including physical therapy, occupational therapy, and speech therapy, plays a vital role in recovery. Patients with persistent deficits may require long-term support and adaptive devices.
Prevention Strategies
1. Managing Risk Factors
- Hypertension Control: Maintain blood pressure below 120/80 mmHg.
- Cholesterol Management: Aim for LDL levels below 70 mg/dL in high-risk individuals.
- Blood Sugar Regulation: Essential for diabetic patients.
2. Regular Health Screenings
Routine health check-ups help in early detection and management of risk factors such as atrial fibrillation and carotid artery stenosis.