Urinary urgency is defined as a sudden, compelling urge to urinate that is difficult to defer. It is a core symptom of overactive bladder (OAB) and can significantly impact quality of life. This symptom may occur alone or alongside increased frequency, nocturia, and urge incontinence. Unlike simple frequent urination due to hydration or diuretics, urinary urgency indicates a potential underlying dysfunction in bladder signaling or control.
The condition affects individuals across all age groups but is more prevalent in older adults and women. Prompt recognition and comprehensive management are essential to prevent complications such as urinary leakage, sleep disturbances, and social withdrawal.
Key Symptoms Associated With Urinary Urgency
Urinary urgency rarely occurs in isolation and is often part of a cluster of symptoms. Common associated manifestations include:
- Sudden, intense need to urinate
- Involuntary urine leakage (urge incontinence)
- Frequent urination (more than eight times in 24 hours)
- Nocturia (waking more than once at night to urinate)
- Anxiety or distress due to unpredictable bladder behavior
In severe cases, the urge may arise even when the bladder is not full, contributing to functional and emotional limitations.
Functional Anatomy of the Urinary System
Urinary urgency arises from disruptions in the coordination between the bladder (detrusor muscle), spinal cord reflexes, and higher brain centers.
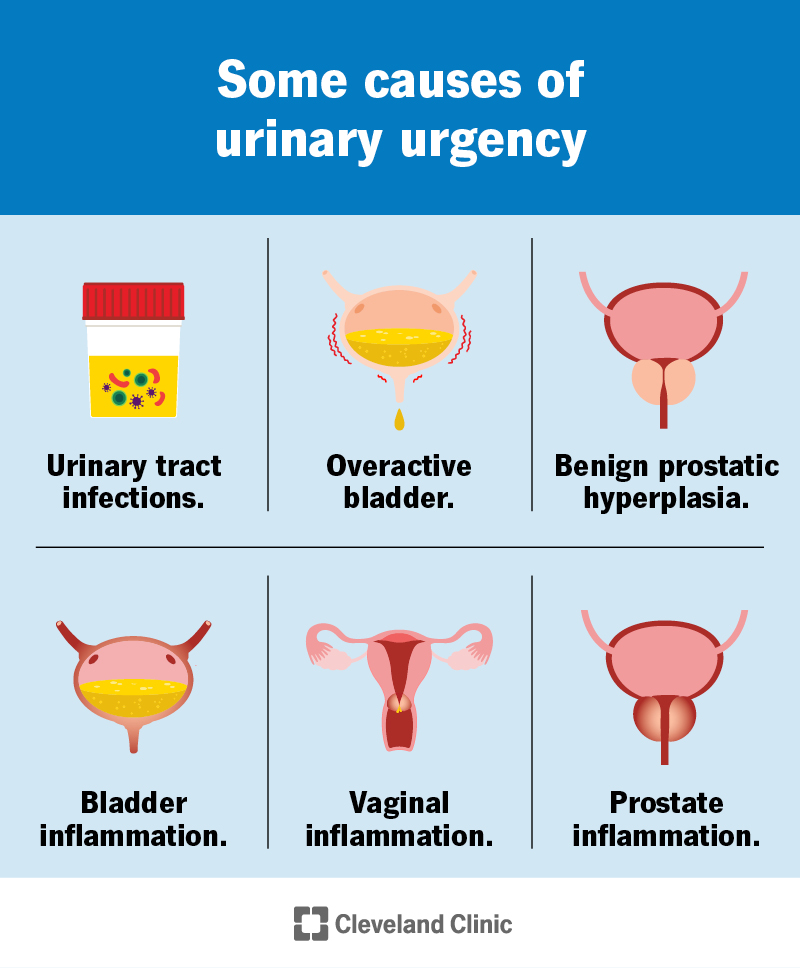
Common Causes of Urinary Urgency
Urinary urgency can be classified based on underlying etiologies. Identification of the root cause is critical for effective treatment.
1. Neurological Disorders
- Multiple sclerosis (MS)
- Parkinson’s disease
- Stroke
- Spinal cord injury
- Diabetic neuropathy
These conditions impair neural pathways controlling bladder function, resulting in detrusor overactivity.
2. Bladder Irritants and Inflammation
- Urinary tract infections (UTIs)
- Interstitial cystitis (painful bladder syndrome)
- Bladder stones or neoplasms
Inflammation or irritation leads to heightened sensory signaling and a lower threshold for urgency.
3. Medications and Substances
- Diuretics (e.g., furosemide)
- Caffeine, alcohol, spicy foods
- Artificial sweeteners
These agents either increase urine output or directly irritate the bladder lining.
4. Pelvic Floor Dysfunction
- Weak pelvic muscles may fail to support the bladder properly.
- Postmenopausal estrogen loss contributes to mucosal thinning and increased urgency.
Diagnostic Approach to Urinary Urgency
A structured evaluation helps delineate the cause and guides treatment.
Clinical History
- Onset, frequency, and severity of urgency
- Association with leakage, pain, or triggers (e.g., sound of water)
- Fluid and caffeine intake
- Comorbid conditions (neurological, metabolic)
Physical Examination
- Abdominal palpation for bladder distention
- Neurological reflexes and tone
- Pelvic exam for atrophy or prolapse in women
- Prostate assessment in men
Diagnostic Investigations
- Urinalysis and urine culture: To exclude infection
- Bladder diary: Logging fluid intake, voiding times, urgency episodes
- Postvoid residual volume measurement: Assesses for incomplete bladder emptying
- Urodynamic testing: Identifies detrusor overactivity and compliance issues
- Imaging (e.g., ultrasound or CT): For stones, masses, or structural anomalies
Evidence-Based Treatment Options for Urinary Urgency
1. Behavioral and Lifestyle Modifications
- Bladder Training: Timed voiding intervals to gradually increase bladder capacity
- Urge Suppression Techniques: Pelvic floor contractions and distraction methods during urgency
- Fluid Regulation: Avoiding large fluid intake before bedtime; reducing diuretics
- Dietary Adjustments: Limiting caffeine, citrus, alcohol, and spicy foods
- Weight Management: Obesity is a risk factor for OAB and urgency
2. Pelvic Floor Muscle Rehabilitation
- Kegel Exercises: Strengthen the muscles that support the urethra
- Biofeedback Training: Visual or auditory feedback to enhance control
- Electrical Stimulation: Stimulates pelvic nerves to improve coordination
3. Pharmacological Management
Antimuscarinics
- Examples: Oxybutynin, tolterodine, solifenacin, darifenacin
- Mechanism: Inhibit muscarinic receptors in bladder smooth muscle
- Side Effects: Dry mouth, constipation, drowsiness
Beta-3 Adrenergic Agonists
- Example: Mirabegron
- Mechanism: Promotes bladder relaxation
- Advantages: Fewer anticholinergic side effects
Topical Estrogen (Women)
- Improves urogenital tissue health and reduces urgency in postmenopausal women
4. Neuromodulation Therapies
- Posterior Tibial Nerve Stimulation (PTNS): Weekly sessions using an electrode near the ankle
- Sacral Neuromodulation (InterStim): Implanted device modulating sacral nerves
5. Botulinum Toxin Injections
- Injected into the bladder wall to block nerve activity
- Reduces urgency and frequency
- May require intermittent self-catheterization in some patients
Special Considerations by Patient Population
Geriatric Patients
- Prefer non-pharmacological options due to polypharmacy risks
- Increased monitoring for falls and cognitive effects of medications
Neurologically Impaired Patients
- Higher reliance on urodynamics and advanced therapies (e.g., Botox, neuromodulation)
- Use of intermittent catheterization if needed
Men with Prostatic Enlargement
- Alpha-blockers may be required in combination with antimuscarinics
- Post-void residual volume must be closely monitored
Prognosis and Long-Term Management
With consistent and individualized treatment, most patients experience significant improvement in urgency symptoms. Long-term strategies include:
- Ongoing bladder training
- Adherence to pharmacologic regimens
- Annual evaluations for therapy adjustments
- Avoiding bladder irritants and adopting healthy voiding habits
Frequently Asked Questions:
Q1. What triggers urinary urgency?
Triggers include bladder irritants, neurological disorders, infections, and certain medications or habits.
Q2. Is urinary urgency always linked to incontinence?
Not always. Some individuals experience urgency without leakage, a condition known as dry OAB.
Q3. Can exercises help with urgency symptoms?
Yes. Pelvic floor exercises significantly improve urgency and frequency in both men and women.
Q4. Are medications effective for everyone?
Most respond well to medications, but some may require combination therapies or procedures.
Q5. Can urinary urgency be prevented?
Prevention includes staying hydrated, avoiding irritants, maintaining pelvic health, and treating UTIs promptly.
Urinary urgency is a complex and often debilitating symptom of overactive bladder and other urological disorders. Through a multifaceted approach involving behavioral therapy, pharmacologic interventions, and advanced procedures, patients can regain control over their bladder health. A comprehensive diagnosis and tailored treatment plan remain the foundation of successful long-term management.