Urinary tract irritation refers to inflammation or sensitivity affecting parts of the urinary system, including the urethra, bladder, and surrounding tissues. This condition often manifests as discomfort, urgency, or burning during urination. It is a common complaint and can stem from infections, chemical exposures, underlying urological conditions, or systemic disorders.
The symptoms may mimic those of a urinary tract infection (UTI), but not all cases are infectious in origin. Proper evaluation and targeted treatment are essential to avoid complications and chronic discomfort.
Key Symptoms of Urinary Tract Irritation
The presentation varies based on severity and underlying cause but typically includes the following irritative voiding symptoms:
- Burning sensation during urination (dysuria)
- Increased urinary frequency and urgency
- Pelvic discomfort or pressure
- Lower abdominal pain
- Nocturia (frequent nighttime urination)
- Cloudy or strong-smelling urine
- Sensation of incomplete bladder emptying
In some cases, symptoms may persist despite negative urine cultures, pointing to non-infectious etiologies.
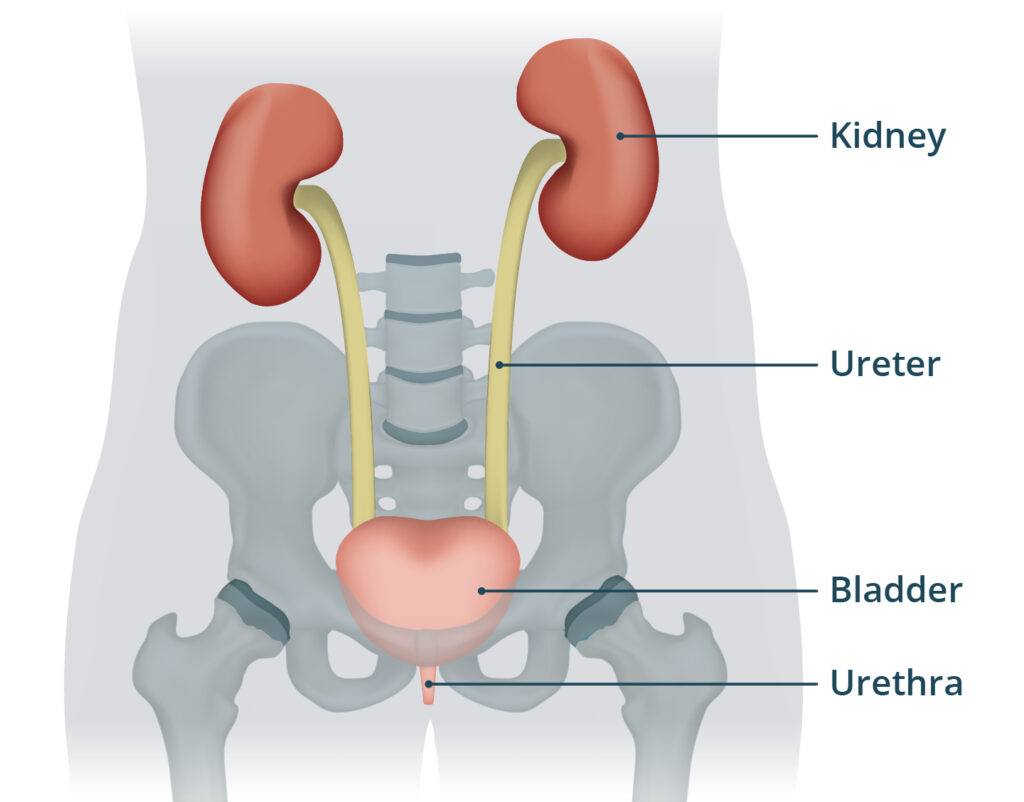
Anatomy of the Urinary Tract: Understanding the Affected Areas
The urinary tract consists of the kidneys, ureters, bladder, and urethra. Irritation commonly affects the lower urinary tract—specifically the bladder and urethra—where inflammation results in discomfort during urination.
Common Causes of Urinary Tract Irritation
1. Infectious Causes
- Urinary Tract Infections (UTIs): Caused by bacteria, primarily Escherichia coli. Infection leads to mucosal inflammation and typical irritative symptoms.
- Sexually Transmitted Infections (STIs): Such as chlamydia, gonorrhea, and herpes can mimic UTI symptoms.
2. Non-Infectious Irritants
- Chemical Irritants: Soaps, bubble baths, douches, or personal hygiene products can trigger mucosal sensitivity.
- Medication Side Effects: Certain antibiotics, chemotherapy agents, and diuretics may irritate the bladder lining.
- Radiation Cystitis: Resulting from pelvic radiation therapy.
- Dietary Irritants: Caffeine, alcohol, citrus fruits, spicy foods, and artificial sweeteners are known bladder irritants.
3. Structural or Functional Abnormalities
- Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS): A chronic inflammatory condition of unknown cause, presenting with ongoing pelvic pain and urinary symptoms.
- Urethral Strictures or Bladder Stones: Cause mechanical irritation to the urethral or bladder lining.
4. Hormonal and Neurological Influences
- Postmenopausal Atrophy: Decreased estrogen can thin the urethral and vaginal mucosa, making it more prone to irritation.
- Overactive Bladder (OAB): Neurological dysfunction leading to urgency and frequency.
Diagnostic Approach to Urinary Tract Irritation
Accurate diagnosis begins with a comprehensive evaluation to identify the underlying cause and rule out serious conditions.
Medical History and Physical Examination
- Detailed symptom review (onset, duration, aggravating factors)
- Pelvic or digital rectal examination
- Review of hygiene products, dietary intake, and medication use
Urinalysis and Urine Culture
- Detect presence of leukocytes, nitrites, hematuria, and bacteria
- Differentiate infectious from non-infectious irritation
Additional Tests
- Cystoscopy: Direct visualization of the bladder lining in chronic or recurrent cases
- Urodynamic Studies: Assess bladder pressure and control in suspected neurological disorders
- Ultrasound or CT Urography: Evaluate for stones, tumors, or anatomical anomalies
Treatment Options for Urinary Tract Irritation
The management strategy is guided by the underlying cause and symptom severity.
Treatment of Infectious Causes
- Antibiotics: Tailored based on urine culture results. Common agents include nitrofurantoin, trimethoprim-sulfamethoxazole, and fosfomycin.
- STI Treatment: Combination antibiotic regimens per guidelines.
Managing Non-Infectious Irritation
- Elimination of Irritants: Discontinuing use of perfumed soaps, douches, and bladder irritant foods.
- Behavioral Therapy: Bladder training and pelvic floor physical therapy for overactive bladder or interstitial cystitis.
- Medications:
- Anticholinergics (e.g., oxybutynin, solifenacin) for bladder overactivity
- Tricyclic antidepressants for pain modulation in interstitial cystitis
- Topical estrogen in postmenopausal women
Supportive Care
- Hydration: Adequate water intake to dilute urine and flush irritants
- Warm Sitz Baths: Alleviate local discomfort
- Avoiding Caffeine and Alcohol: Reduce bladder hypersensitivity
Preventing Urinary Tract Irritation
Adopting healthy habits can significantly reduce the risk of urinary tract irritation.
- Wipe front to back to prevent bacterial spread
- Urinate before and after sexual activity
- Avoid prolonged holding of urine
- Wear breathable cotton underwear
- Limit bladder irritants in the diet
Chronic Irritation and When to Seek Specialist Care
Persistent symptoms despite treatment necessitate urology or gynecology referral. Conditions like interstitial cystitis, recurrent UTIs, or bladder malignancies require expert management. Early specialist intervention helps prevent long-term complications and improves quality of life.
Frequently Asked Questions:
Q1. Can urinary tract irritation occur without infection?
Yes. Non-infectious factors like chemicals, foods, or underlying bladder disorders often cause irritation without infection.
Q2. What foods commonly irritate the urinary tract?
Citrus fruits, spicy foods, caffeine, chocolate, tomatoes, and artificial sweeteners are common triggers.
Q3. Is urinary tract irritation the same as a UTI?
Not always. While UTIs cause irritation, not all irritation is due to infection.
Q4. How is bladder irritation treated?
Treatment includes removing triggers, hydration, medications, and addressing underlying causes like IC or OAB.
Q5. Does urinary tract irritation go away on its own?
Mild cases may resolve with lifestyle changes, but persistent symptoms require medical evaluation.
Urinary tract irritation is a multifaceted condition with diverse etiologies ranging from infections to lifestyle-related triggers. Timely recognition and a structured diagnostic approach are crucial for identifying the root cause. With tailored treatment strategies and preventative measures, most individuals can achieve substantial symptom relief and restore optimal urinary tract health.