Urinary retention is a urological condition characterized by the inability to empty the bladder completely or at all, despite the urge to urinate. It is classified into two main types: acute urinary retention, which presents suddenly and is a medical emergency, and chronic urinary retention, which develops gradually and may remain undetected for a prolonged period. Left untreated, this condition can result in severe complications such as bladder damage, urinary tract infections (UTIs), and kidney impairment.
Types of Urinary Retention
Acute Urinary Retention
- Definition: Sudden and painful inability to urinate.
- Onset: Rapid and requires emergency intervention.
- Symptoms: Severe lower abdominal pain, urgency without output, distended bladder.
Chronic Urinary Retention
- Definition: Gradual inability to empty the bladder fully.
- Onset: Often asymptomatic in early stages.
- Symptoms: Weak urine stream, hesitancy, frequent urination, nocturia, and sensation of incomplete emptying.
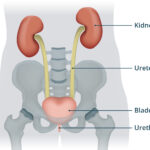
Anatomical Overview: Bladder Function and Urination Process
The bladder functions as a reservoir for urine, coordinated by the detrusor muscle and a series of neurological signals from the brain and spinal cord. The urethral sphincters control the flow of urine during micturition. Urinary retention arises when any part of this complex system is disrupted.
Causes of Urinary Retention
Urinary retention can result from mechanical obstruction, neurological dysfunction, pharmacological effects, or infections and inflammation. A thorough understanding of these causes is essential for accurate diagnosis and treatment.
Obstructive Causes
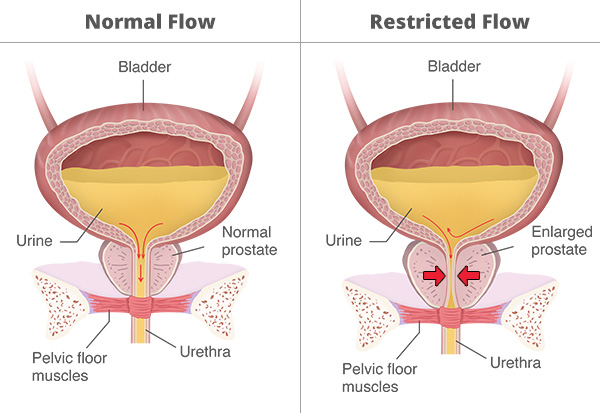
- Benign Prostatic Hyperplasia (BPH): Common in aging males; enlarged prostate compresses the urethra.
- Urethral Strictures: Narrowing of the urethra due to injury or infection.
- Bladder Stones or Tumors: Obstruct the urethral outlet.
- Pelvic Masses: Such as uterine fibroids or cancers impinging on urinary structures.
Neurological Causes
- Spinal Cord Injuries: Disruption in the micturition reflex arc.
- Multiple Sclerosis: Demyelination affecting bladder control.
- Parkinson’s Disease and Stroke: Impaired central regulation of voiding.
Functional and Pharmacologic Causes
- Detrusor Underactivity: Age-related or idiopathic.
- Medications: Anticholinergics, opioids, sympathomimetics, and certain antihistamines can impair bladder contraction.
- Postoperative Retention: Especially after surgeries involving anesthesia or the pelvic region.
Inflammatory Causes
- Prostatitis: Inflammation of the prostate.
- Urinary Tract Infections: Swelling and irritation impair bladder function.
Clinical Presentation and Symptoms
The symptoms vary based on the type and underlying cause. Acute cases are dramatic and painful, while chronic cases often go unnoticed until complications develop.
Acute Retention Symptoms:
- Sudden inability to void
- Intense suprapubic pain
- Palpable bladder distension
- Anxiety and discomfort
Chronic Retention Symptoms:
- Slow urinary stream
- Hesitancy
- Intermittent flow
- Increased frequency and nocturia
- Incontinence due to overflow
Diagnosis of Urinary Retention
A detailed diagnostic approach is vital to distinguish between acute and chronic forms and identify the root cause.
Medical History and Physical Examination
- History of urinary symptoms, surgeries, medications, and neurological conditions.
- Digital rectal examination (DRE) to assess prostate size.
- Pelvic exam in women to identify anatomical abnormalities.
Bladder Ultrasound
- Post-void residual (PVR): Measures residual urine volume after voiding.
- PVR >100 mL is suggestive of urinary retention.
Urodynamic Studies
- Assess detrusor muscle function and bladder compliance.
- Useful in identifying detrusor underactivity or obstruction.
Cystoscopy
- Direct visualization of the urethra and bladder for strictures, tumors, or stones.
Neurological Evaluation
- MRI or CT scan if a spinal cord lesion or brain pathology is suspected.
Management and Treatment Strategies
Treatment of urinary retention depends on the underlying etiology and whether the condition is acute or chronic.
Immediate Management of Acute Urinary Retention
- Urethral Catheterization: Rapid decompression of the bladder.
- Suprapubic Catheterization: Used when urethral catheterization is contraindicated.
- Monitor for post-obstructive diuresis and renal function.
Long-Term Management of Chronic Retention
Medical Therapy
- Alpha-Blockers: Tamsulosin or alfuzosin to relax prostatic and bladder neck smooth muscle.
- 5-Alpha Reductase Inhibitors: Finasteride or dutasteride to reduce prostate size in BPH.
- Cholinergic Agonists: Such as bethanechol in selected cases of detrusor underactivity.
Intermittent Self-Catheterization (ISC)
- Preferred method for managing chronic retention due to detrusor weakness or neurogenic causes.
Surgical Intervention
- Transurethral Resection of the Prostate (TURP): Standard treatment for BPH-induced retention.
- Urethral Dilation or Urethrotomy: For urethral strictures.
- Sacral Neuromodulation: For neurogenic bladder dysfunction.
Complications of Untreated Urinary Retention
Failure to address urinary retention can result in severe medical consequences:
- Hydronephrosis and Renal Failure: Due to back pressure on kidneys.
- Recurrent UTIs
- Bladder Decompensation: Permanent loss of detrusor muscle function.
- Overflow Incontinence
Preventive Strategies and Patient Education
- Early recognition of symptoms in high-risk individuals (e.g., elderly males with BPH)
- Avoid unnecessary anticholinergic medications in susceptible patients
- Monitor post-operative urinary function in surgical patients
- Encourage timely and complete voiding habits
Urinary retention is a multifactorial condition with significant implications for renal and bladder health. Prompt recognition and an individualized management approach—ranging from catheterization and medical therapy to surgical correction—are key to restoring normal urinary function and improving patient outcomes. A multidisciplinary evaluation ensures accurate diagnosis and effective long-term care.