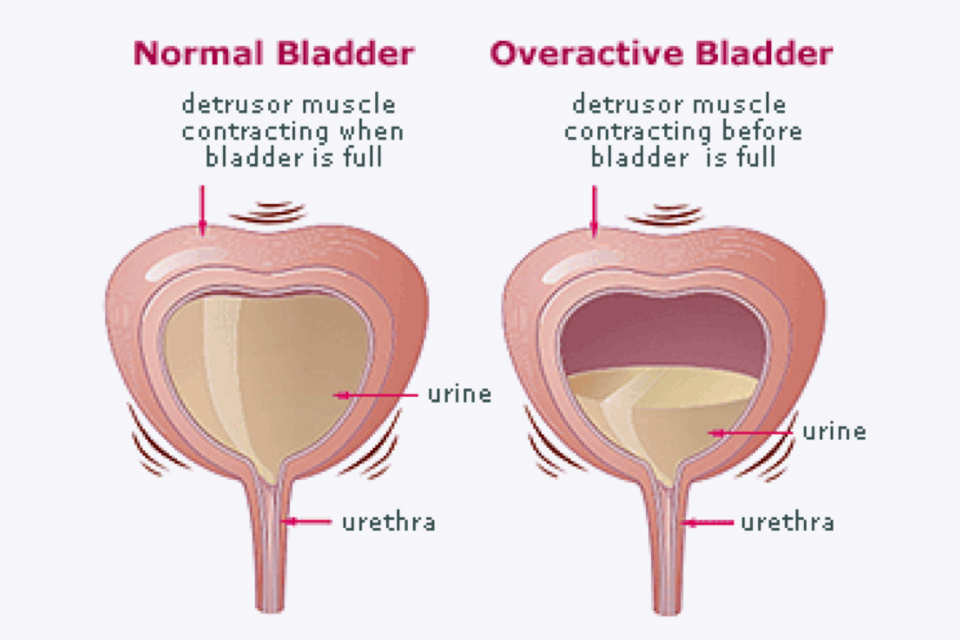
Detrusor overactivity is a urodynamic condition characterized by involuntary contractions of the detrusor muscle during the bladder filling phase. These contractions can lead to urinary urgency, frequency, nocturia, and urge urinary incontinence. As one of the primary causes of overactive bladder (OAB), detrusor overactivity significantly impairs quality of life and affects both men and women, particularly with advancing age or in the presence of neurological disorders.
Understanding the Detrusor Muscle and Its Role in Micturition
The detrusor muscle is the smooth muscle layer of the bladder wall responsible for contractions that expel urine. In a healthy bladder, it remains relaxed during the filling phase and contracts voluntarily during voiding. In detrusor overactivity, this regulation fails, and involuntary contractions occur, often leading to sudden and uncontrollable urges to urinate.
Causes and Risk Factors of Detrusor Overactivity
Detrusor overactivity can arise from multiple underlying factors, both idiopathic and neurogenic. Identifying the cause is essential for effective management.
Neurological Causes
- Multiple Sclerosis
- Parkinson’s Disease
- Stroke
- Spinal Cord Injury
- Brain Tumors
These conditions disrupt the neural pathways involved in bladder control, resulting in detrusor hyperactivity.
Idiopathic Causes
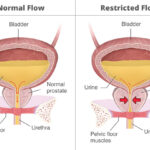
In many individuals, detrusor overactivity occurs without identifiable neurological abnormalities. Common contributing factors include:
- Aging: Degenerative changes in bladder innervation and detrusor muscle sensitivity
- Bladder Outlet Obstruction: Secondary to benign prostatic hyperplasia (BPH)
- Bladder Irritation: Due to recurrent urinary tract infections or bladder stones
- Post-Menopausal Changes: Estrogen deficiency affecting bladder and urethral tissues
Clinical Presentation of Urinary Incontinence Due to Detrusor Overactivity
Patients typically report:
- Urgency: A sudden, compelling need to void
- Frequency: Voiding more than eight times per day
- Nocturia: Waking up more than once at night to urinate
- Urge Incontinence: Involuntary urine leakage following an intense urge to void
These symptoms may occur in isolation or conjunction and often result in significant distress, embarrassment, and limitation of daily activities.
Diagnostic Evaluation
Accurate diagnosis requires a thorough clinical assessment supported by specialized urodynamic tests.
Medical History and Physical Examination
- Review of urinary symptoms, medication use, and neurological status
- Digital rectal exam (in men) and pelvic exam (in women) to assess for pelvic organ prolapse or prostate enlargement
Urinalysis and Culture
- Rules out urinary tract infection or hematuria
Bladder Diary
- Tracks voiding patterns, frequency, and volume for several days
Urodynamic Studies
The definitive diagnostic tool:
- Cystometry: Measures bladder pressure and capacity during filling
- Involuntary Detrusor Contractions: Confirm the diagnosis of detrusor overactivity
- Pressure-Flow Studies: Assess detrusor pressure during voiding
Cystoscopy
- May be indicated if hematuria or suspicion of bladder pathology exists
Treatment Options for Detrusor Overactivity-Related Urinary Incontinence
Effective treatment requires a combination of behavioral, pharmacologic, and interventional strategies tailored to symptom severity and patient profile.
Behavioral Interventions
- Bladder Training: Gradual extension of intervals between voiding
- Pelvic Floor Muscle Exercises: Enhance urethral resistance and bladder control
- Fluid Management: Regulate intake of caffeine and bladder irritants
Pharmacological Therapy
Medications remain the mainstay of first-line treatment:
Antimuscarinics
- Examples: Oxybutynin, Tolterodine, Solifenacin
- Mechanism: Block acetylcholine at muscarinic receptors, reducing detrusor contractions
- Side Effects: Dry mouth, constipation, blurred vision
Beta-3 Adrenergic Agonists
- Example: Mirabegron
- Mechanism: Activates β3 receptors, promoting bladder relaxation
- Benefits: Better tolerability, especially in elderly patients
Topical Vaginal Estrogen
- Useful for post-menopausal women with urogenital atrophy contributing to symptoms
Neuromodulation Therapies
Indicated for refractory detrusor overactivity:
- Sacral Neuromodulation (SNS): Electrical stimulation of sacral nerves (S3) modulates bladder activity
- Posterior Tibial Nerve Stimulation (PTNS): Less invasive, done via peripheral nerve access
Botulinum Toxin Injections
- Mechanism: Inhibits acetylcholine release, relaxing the detrusor muscle
- Efficacy: High success rates in reducing incontinence episodes
- Considerations: Risk of urinary retention; requires periodic reinjection
Surgical Options
Reserved for severe, unresponsive cases:
- Augmentation Cystoplasty: Expands bladder capacity using a segment of intestine
- Urinary Diversion: Bypasses the bladder entirely in extreme cases
Managing Detrusor Overactivity in Special Populations
Elderly Patients
- Prefer agents with minimal cognitive side effects (e.g., mirabegron)
- Monitor for polypharmacy and anticholinergic burden
Patients with Neurological Disorders
- Require regular urodynamic monitoring
- May benefit more from intermittent catheterization or botulinum toxin therapy
Long-Term Outlook and Quality of Life
Urinary incontinence due to detrusor overactivity, though chronic in many cases, can be effectively managed. Multimodal therapy tailored to the individual leads to significant improvement in symptoms and quality of life. Early intervention, lifestyle modification, and adherence to therapy are critical in preventing complications such as recurrent infections or social withdrawal.
Detrusor overactivity is a central cause of urge urinary incontinence and overactive bladder syndrome. A structured approach to diagnosis and individualized treatment ensures optimal outcomes. With evolving therapies, including neuromodulation and botulinum toxin injections, most patients can achieve substantial relief from symptoms and regain control over their urinary function.