Urinary incontinence (UI) refers to the involuntary leakage of urine, a condition that affects millions of individuals globally, particularly women and older adults. While it may seem like an unavoidable consequence of aging or childbirth, UI is a treatable medical condition with a wide range of management strategies. Understanding the different forms and underlying causes is essential to providing targeted and effective care.
Types of Urinary Incontinence
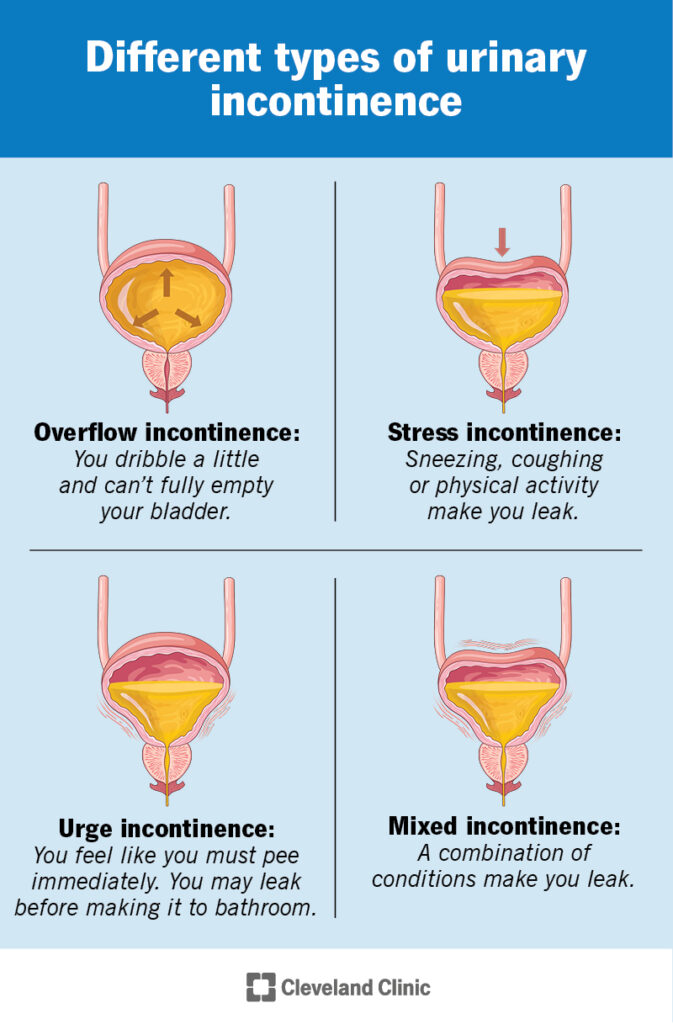
Stress Incontinence
Stress incontinence occurs when physical movement or activity — such as coughing, sneezing, or exercising — puts pressure on the bladder, leading to leakage. It is most commonly caused by weakened pelvic floor muscles, often due to pregnancy, childbirth, or menopause.
Urge Incontinence
Also known as overactive bladder (OAB), urge incontinence is characterized by a sudden and intense urge to urinate, followed by involuntary loss of urine. It is associated with involuntary bladder muscle contractions.
Overflow Incontinence
This type results from an inability to empty the bladder completely, leading to frequent or constant dribbling of urine. It is often linked to conditions such as diabetes, spinal injury, or prostate enlargement.
Functional Incontinence
Functional incontinence arises when physical or mental impairments prevent a person from reaching the toilet in time. It is commonly observed in elderly patients or those with neurological disorders.
Mixed Incontinence
A combination of stress and urge incontinence, mixed incontinence is common among women and requires a multifaceted approach for treatment.
Causes and Risk Factors
A thorough understanding of the root causes helps in designing effective interventions:
- Aging: Muscle tone reduction and decreased bladder capacity.
- Pregnancy and Childbirth: Pelvic floor weakening and nerve damage.
- Menopause: Estrogen deficiency impacting urinary tract health.
- Prostate Issues: Enlargement or post-surgical effects in men.
- Neurological Conditions: Parkinson’s, multiple sclerosis, or stroke.
- Obesity: Increased abdominal pressure affecting bladder control.
- Medications: Diuretics or sedatives contributing to bladder dysfunction.
Diagnosing Urinary Incontinence
Accurate diagnosis is critical for effective treatment. Diagnostic procedures include:
- Urinalysis: Detects infection or traces of blood.
- Bladder Diary: Tracks frequency, volume, and leakage episodes.
- Post-Void Residual Measurement: Assesses remaining urine after urination.
- Urodynamic Testing: Evaluates bladder pressure and flow.
- Cystoscopy: Visual inspection of the urinary tract using a scope.
Treatment Options for Urinary Incontinence
Lifestyle and Behavioral Therapies
- Pelvic Floor Exercises (Kegels): Strengthen the muscles controlling urination.
- Bladder Training: Increase intervals between urination.
- Dietary Modifications: Avoiding caffeine, alcohol, and acidic foods.
- Weight Loss: Reducing abdominal pressure on the bladder.
Medical and Pharmacological Treatments
- Anticholinergics: Reduce bladder spasms (e.g., oxybutynin, tolterodine).
- Beta-3 Adrenergic Agonists: Improve bladder capacity and reduce urgency.
- Topical Estrogen: Helps restore vaginal and urethral tissue in postmenopausal women.
- Alpha-blockers: Aid in emptying the bladder in men with prostate issues.
Non-Surgical Interventions
- Pessary Devices: Support pelvic organs and reduce leakage.
- Urethral Inserts: Temporary devices for women to prevent leakage during activities.
- Nerve Stimulation (Tibial or Sacral): Modulates nerve signals to the bladder.
Surgical Treatments
- Sling Procedures: Support urethra with synthetic or biological materials.
- Bladder Neck Suspension: Lifts the bladder neck for better control.
- Artificial Urinary Sphincter: Primarily used in male patients post-prostate surgery.
- Prostate Surgery: Treats overflow incontinence due to BPH.
Preventing Urinary Incontinence
Preventative strategies can significantly reduce the risk of UI:
- Early Pelvic Floor Training: Especially during pregnancy or post-childbirth.
- Maintain Healthy Weight: Obesity is a major risk factor.
- Smoking Cessation: Smoking increases coughing and risk of stress incontinence.
- Regular Physical Activity: Improves overall muscle tone and bladder health.
- Avoid Constipation: High-fiber diets and hydration support bowel health, reducing bladder pressure.
Living with Urinary Incontinence
Emotional and Social Impact
UI can affect mental health, self-esteem, and social engagement. Addressing these impacts through counseling and support groups is crucial.
Incontinence Products and Lifestyle Aids
- Absorbent Pads and Protective Garments
- Waterproof Bedding and Mattress Covers
- Portable Toilets and Timed Voiding Reminders
Professional Support
Consulting urologists, urogynecologists, or pelvic floor therapists ensures a comprehensive and personalized treatment plan.
Urinary incontinence, while common, is not an inevitable consequence of aging or childbirth. With advancements in diagnosis and treatment, individuals suffering from UI can regain control and significantly improve their quality of life. Early intervention, lifestyle changes, and expert-guided care are the cornerstones of effective management. Through informed decision-making and proactive healthcare, urinary incontinence can be effectively addressed and often resolved.