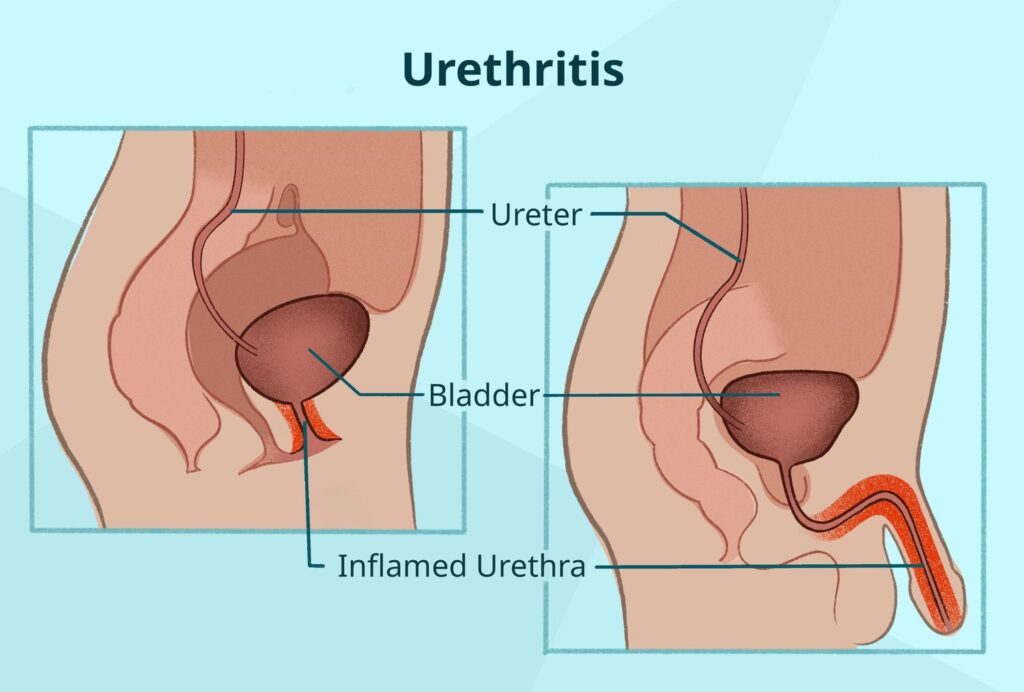
Urethritis refers to the inflammation of the urethra, the thin tube responsible for transporting urine from the bladder to the outside of the body. This condition can affect individuals of any gender or age and is commonly caused by infections, irritants, or trauma. Urethritis is categorized into gonococcal urethritis (caused by Neisseria gonorrhoeae) and non-gonococcal urethritis (NGU), typically caused by other pathogens such as Chlamydia trachomatis, Mycoplasma genitalium, and Ureaplasma urealyticum.
Common Symptoms of Urethritis
Urethritis manifests differently depending on the underlying cause. However, the most frequent signs include:
- Burning sensation during urination (dysuria)
- Urethral discharge (clear, white, yellow, or green)
- Itching or irritation inside the penis or around the vaginal opening
- Frequent urge to urinate
- Pain during intercourse
- Blood in urine or semen (less common)
Gender-Specific Symptoms
- Men often experience visible urethral discharge and penile discomfort.
- Women may experience vaginal irritation, pelvic pain, and may confuse urethritis with cystitis due to overlapping symptoms.
Causes and Risk Factors
Infectious Causes
- Sexually Transmitted Infections (STIs):
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Mycoplasma genitalium
- Trichomonas vaginalis
- Herpes Simplex Virus (HSV)
- Non-Sexually Transmitted Pathogens:
- Escherichia coli
- Ureaplasma urealyticum
Non-Infectious Causes
- Chemical irritants (e.g., spermicides, soaps, lubricants)
- Physical trauma (e.g., catheterization, vigorous sexual activity)
- Autoimmune disorders (e.g., Reiter’s syndrome)
Risk Factors
- Multiple sexual partners
- Unprotected intercourse
- Previous history of STIs
- Poor hygiene
- Compromised immune system
Diagnostic Evaluation
Early and accurate diagnosis of urethritis is critical to prevent complications such as infertility, epididymitis, or pelvic inflammatory disease (PID).
Clinical Examination
- Assessment of medical and sexual history
- Physical examination of genitalia
Laboratory Testing
- Urine Analysis: First-void urine tested for white blood cells and pathogens
- Urethral Swab: Microscopy, culture, and nucleic acid amplification tests (NAATs)
- STI Screening: Includes gonorrhea, chlamydia, trichomoniasis, and herpes
Effective Treatment Options
Treatment depends on the underlying cause and pathogen identified. Antibiotic therapy remains the primary intervention for infectious urethritis.
Gonococcal Urethritis
- Ceftriaxone 500 mg IM single dose
- Plus Doxycycline 100 mg orally twice daily for 7 days (if chlamydia not excluded)
Non-Gonococcal Urethritis (NGU)
- Doxycycline 100 mg orally twice daily for 7 days
- Alternatives: Azithromycin 1 g orally in a single dose (less preferred due to resistance)
Persistent or Recurrent Cases
- Consider Mycoplasma genitalium and treat with:
- Moxifloxacin 400 mg daily for 7–14 days
- Evaluate for reinfection or inadequate partner treatment
Symptomatic Management
- Analgesics (e.g., ibuprofen)
- Increased fluid intake
- Avoidance of irritants and sexual activity until cured
Prevention and Partner Management
Preventive Measures
- Use of barrier contraception (condoms)
- Regular STI screening for sexually active individuals
- Limiting number of sexual partners
- Avoiding irritant hygiene products
Partner Notification and Treatment
- All recent sexual partners (within 60 days) should be informed, tested, and treated
- Abstinence is recommended until all parties have completed treatment
Potential Complications
If left untreated or inadequately treated, urethritis can result in:
- Male Complications:
- Epididymitis
- Prostatitis
- Urethral stricture
- Female Complications:
- Pelvic inflammatory disease (PID)
- Infertility
- Ectopic pregnancy
- Systemic Effects:
- Reactive arthritis
- Disseminated gonococcal infection
Prognosis and Long-Term Outlook
When treated promptly and appropriately, urethritis typically resolves without lasting effects. However, delayed treatment increases the risk of chronic inflammation and complications. Regular follow-ups and partner management are essential to ensure full recovery and prevent reinfection.
Frequently Asked Questions:
What is the most common cause of urethritis?
Chlamydia trachomatis and Neisseria gonorrhoeae are the leading causes of urethritis globally.
Can urethritis go away on its own?
Infectious urethritis rarely resolves without antibiotics and may lead to serious complications if untreated.
How long does it take to recover from urethritis?
With proper treatment, symptoms often improve within 2–3 days and resolve completely in 7–10 days.
Is urethritis contagious?
Yes, if caused by infectious agents, urethritis can be transmitted through sexual contact.
Can women get urethritis?
Yes, although symptoms in women may be less specific, they are equally susceptible to urethral infections.
Urethritis is a prevalent condition with potentially serious consequences if neglected. Prompt diagnosis, effective treatment, and preventive strategies are essential to managing this condition successfully. Both healthcare providers and patients must prioritize awareness and adherence to treatment protocols to ensure complete recovery and prevent transmission.