Upper respiratory streptococcal infection, primarily caused by Streptococcus pyogenes (Group A Streptococcus or GAS), remains a significant contributor to global morbidity. This infection often presents as streptococcal pharyngitis (strep throat) but may also involve the tonsils, sinuses, and middle ear. If not adequately treated, it may progress to severe complications, including rheumatic fever and post-streptococcal glomerulonephritis.
Pathogenesis and Etiology of Streptococcal URI
Streptococcus pyogenes is a Gram-positive, beta-hemolytic bacterium that colonizes the oropharynx and is transmitted via respiratory droplets. Upon entry, it adheres to epithelial cells through fibronectin-binding proteins and evades the immune response using virulence factors such as M protein, streptolysins, and exotoxins.
Common Types of Upper Respiratory Streptococcal Infections
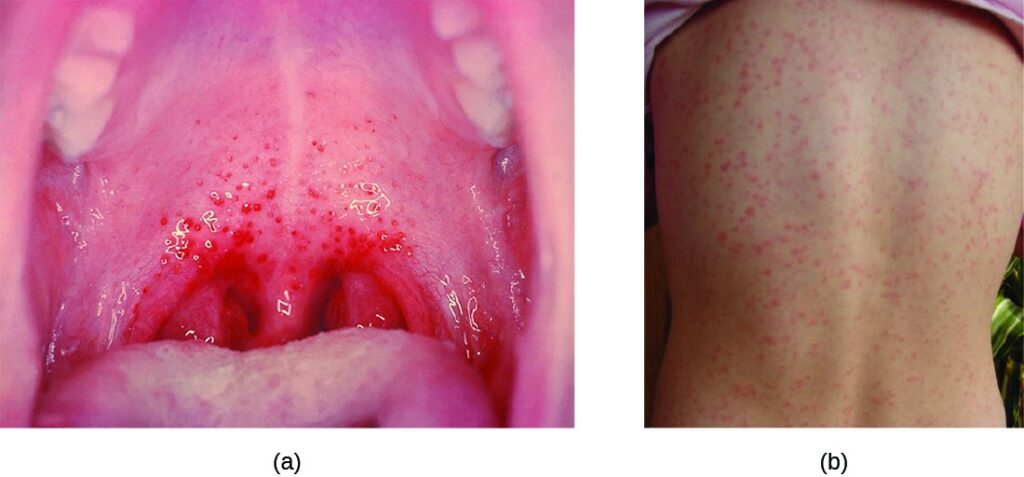
1. Streptococcal Pharyngitis (Strep Throat)
The most prevalent manifestation, it typically affects school-aged children.
Symptoms:
- Sudden sore throat
- Painful swallowing
- Fever (>38.5°C)
- Swollen, tender cervical lymph nodes
- Tonsillar exudate
- Absence of cough
2. Tonsillitis
Characterized by inflamed, red, and swollen tonsils often with white patches or pus.
3. Sinusitis and Otitis Media
Less commonly, streptococcus can cause upper respiratory sinus and ear infections, especially following a viral illness.
Modes of Transmission and Risk Factors
The bacterium spreads via respiratory droplets, direct contact, or contaminated surfaces. Peak incidence occurs in winter and early spring.
Key Risk Factors:
- Close contact in schools or daycare
- Poor hygiene practices
- Crowded living conditions
- Recent exposure to an infected person
- Immunocompromised states
Diagnostic Approach to Streptococcal URTI
Accurate diagnosis differentiates GAS from viral URTIs, avoiding unnecessary antibiotic use.
Diagnostic Tools:
- Rapid Antigen Detection Test (RADT): Results within minutes; high specificity.
- Throat Culture: Gold standard; detects even low bacterial loads. Results in 24–48 hours.
- Centor Criteria (Modified): Clinical FeatureScoreFever (>38°C)+1Tonsillar exudates+1Tender anterior nodes+1Absence of cough+1Age 3–14 years+1Age ≥45 years-1
A score of ≥3 warrants RADT or empirical treatment.
Treatment Protocols for Streptococcal Infections
Prompt treatment minimizes symptom duration, transmission, and post-infectious complications.
First-Line Antibiotics:
| Drug | Dosage and Notes |
|---|---|
| Penicillin V | 500 mg BID for 10 days (adults) |
| Amoxicillin | 500 mg TID for 10 days |
| Benzathine Penicillin G | IM single dose (especially for compliance) |
| Cephalexin | For mild penicillin allergy |
| Azithromycin or Clindamycin | For severe penicillin allergy |
Note: GAS is universally sensitive to penicillin.
Symptomatic Relief:
- Paracetamol or ibuprofen for pain and fever
- Saltwater gargles
- Hydration and rest
Complications from Untreated Streptococcal Infections
Failure to treat can lead to immune-mediated and invasive complications.
Non-Suppurative:
- Acute Rheumatic Fever
- Post-streptococcal Glomerulonephritis
- Scarlet Fever
- PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders)
Suppurative:
- Peritonsillar abscess
- Otitis media
- Sinusitis
- Cervical lymphadenitis
Prevention Strategies
1. Personal Hygiene
- Frequent handwashing
- Avoiding sharing utensils or drinks
- Covering mouth and nose while coughing or sneezing
2. Isolation and Early Treatment
- Infected individuals should avoid school/work until 24 hours after starting antibiotics.
3. No Vaccine Available for GAS
As of now, no licensed vaccine exists against Group A Streptococcus, making hygiene and timely diagnosis the primary defense.
Public Health Importance
Streptococcal URTIs contribute substantially to antibiotic prescriptions. Overuse promotes resistance in co-colonizing organisms, even though GAS remains sensitive to penicillin. Public awareness, diagnostic stewardship, and timely treatment are vital for reducing complications and transmission.
Upper respiratory streptococcal infections, notably streptococcal pharyngitis, are common, highly contagious, and potentially serious. Caused by Streptococcus pyogenes, these infections require prompt diagnosis using RADT or culture and effective antibiotic therapy. Preventive measures and public health awareness are key to minimizing disease spread and the risk of long-term sequelae.