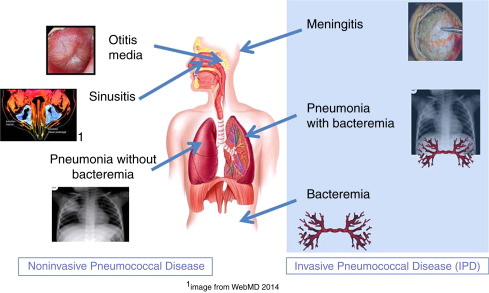
Streptococcus pneumoniae, commonly known as pneumococcus, remains a leading cause of upper respiratory tract infections (URTIs), particularly in vulnerable populations such as young children, the elderly, and immunocompromised individuals. Although frequently carried asymptomatically, this pathogen has the capacity to cause a spectrum of diseases, from mild sinusitis to severe pneumonia and invasive pneumococcal disease (IPD).
Overview of Streptococcus pneumoniae and Its Role in URTIs
Streptococcus pneumoniae is a Gram-positive, encapsulated diplococcus that colonizes the human nasopharynx, particularly in early childhood. The asymptomatic colonization serves as the reservoir for person-to-person transmission and potential progression to disease.
Upper respiratory pneumococcal infections primarily involve the sinuses, middle ear, and bronchial passages, with occasional extension into the lower respiratory tract or bloodstream.
Pathophysiology of Pneumococcal Upper Respiratory Infection
The initiation of infection typically follows viral upper respiratory illnesses that compromise mucosal defenses. Pneumococci adhere to epithelial cells and evade immune clearance via capsular polysaccharides, pneumolysin, and other virulence factors.
Key virulence factors such as pneumolysin and autolysins contribute to epithelial damage and inflammation, enhancing bacterial proliferation and spread.
Transmission and Risk Factors
Transmission occurs via respiratory droplets, often in crowded settings or among individuals with close contact. Carriage rates are highest among children under five and can reach up to 60% in daycare populations.
Major Risk Factors:
- Recent viral respiratory infection (e.g., influenza, RSV)
- Age <5 years or >65 years
- Chronic pulmonary disease (e.g., COPD, asthma)
- Immunosuppression or HIV infection
- Cigarette smoke exposure
- Absence of pneumococcal vaccination
Clinical Presentation of Pneumococcal Upper Respiratory Infections
While presentations vary by site of infection, pneumococcal URTIs generally present with acute onset symptoms.
Common Manifestations:
| Condition | Key Symptoms |
|---|---|
| Acute sinusitis | Facial pain, purulent nasal discharge, nasal congestion |
| Otitis media | Ear pain, hearing loss, fever, irritability in children |
| Pharyngitis | Sore throat, mild fever, swollen lymph nodes |
| Bronchitis | Persistent cough, chest discomfort, low-grade fever |
Systemic signs such as high fever, lethargy, or chills may suggest a transition to invasive disease and warrant urgent evaluation.
Diagnostic Evaluation
Accurate diagnosis is essential to distinguish pneumococcal URTIs from viral or other bacterial etiologies.
Diagnostic Modalities:
- Nasopharyngeal swab culture or PCR: Confirms presence of S. pneumoniae
- Sinus aspiration (rarely used): For culture in refractory cases
- Tympanocentesis: Diagnostic in otitis media with effusion
- Chest X-ray: To exclude lower respiratory tract involvement
- Complete blood count (CBC): Leukocytosis may indicate bacterial infection
- C-reactive protein (CRP): Elevated in bacterial URTIs
Rapid antigen tests (e.g., urinary antigen detection) are reserved for more severe or systemic manifestations.
Treatment Strategies for Upper Respiratory Pneumococcal Infection
The cornerstone of treatment is prompt initiation of appropriate antibiotics, along with symptomatic relief.
First-Line Antibiotics:
| Drug | Indication |
|---|---|
| Amoxicillin | First-line for uncomplicated infections |
| Amoxicillin-Clavulanate | In resistant or recurrent cases |
| Cefuroxime or Cefpodoxime | Second-line options |
| Levofloxacin or Moxifloxacin | For beta-lactam-allergic adults |
| Clindamycin or Azithromycin | Macrolide-sensitive cases |
Treatment duration typically ranges from 5 to 10 days depending on the site and severity of infection.
Adjunctive Therapies:
- Nasal decongestants (for sinusitis)
- Analgesics (for ear or facial pain)
- Antipyretics (for fever management)
Preventive Measures and Vaccination
Vaccination is the most effective tool in reducing incidence, severity, and transmission of pneumococcal disease.
Available Vaccines:
- PCV13 (Pneumococcal Conjugate Vaccine): For children <5 years and high-risk adults
- PPSV23 (Pneumococcal Polysaccharide Vaccine): For adults ≥65 years and certain high-risk populations
Schedule:
- Children: 4-dose PCV13 series (2, 4, 6, and 12–15 months)
- Adults ≥65 years: One dose PCV followed by PPSV23
Complications and Disease Progression
Although many pneumococcal URTIs resolve with treatment, some may progress to more serious conditions if inadequately managed.
Potential Complications:
- Acute mastoiditis
- Bacterial meningitis
- Pneumonia
- Bacteremia and sepsis
- Hearing loss (from recurrent otitis media)
Vigilance is warranted in high-risk individuals, especially those presenting with systemic signs or non-resolving symptoms.
Public Health Considerations
Mass pneumococcal vaccination campaigns have led to a marked decline in invasive pneumococcal disease, but URTIs caused by non-vaccine serotypes persist. Surveillance of serotype prevalence and antimicrobial resistance patterns remains crucial for public health planning.
Antimicrobial Stewardship:
To reduce resistance, antibiotics should be used judiciously, with preference for narrow-spectrum agents unless broader coverage is clinically justified.
Upper respiratory pneumococcal infection remains a significant cause of morbidity across age groups, particularly in unvaccinated and immunocompromised individuals. Early diagnosis, appropriate antibiotic therapy, and vaccination are central to controlling the disease burden. Proactive management, including addressing predisposing viral infections and risk factors, is essential to prevent progression and community spread.