Upper gastrointestinal (GI) bleeding is a potentially life-threatening condition that originates proximal to the ligament of Treitz, encompassing bleeding from the esophagus, stomach, or duodenum. Prompt recognition, risk stratification, and targeted intervention are imperative to reduce morbidity, mortality, and recurrence.
Etiology and Common Causes of Upper GI Bleed
The etiology of upper GI bleeding varies with age, comorbidities, and regional prevalence of gastrointestinal disorders. The most common causes include:
1. Peptic Ulcer Disease (PUD)
- The leading cause, accounting for up to 60% of non-variceal bleeds.
- Related to Helicobacter pylori infection or NSAID use.
- Duodenal ulcers are more common than gastric ulcers.
2. Esophageal Varices
- Result from portal hypertension, commonly seen in cirrhosis.
- High risk of rapid, massive hemorrhage.
3. Mallory-Weiss Tear
- Mucosal laceration at the gastroesophageal junction due to forceful vomiting or retching.
- Typically presents with brisk hematemesis.
4. Gastric and Duodenal Erosions
- Superficial mucosal damage, often due to alcohol, stress, or medications.
- Usually less severe but recurrent.
5. Malignancy
- Gastric or esophageal cancer may cause occult or overt bleeding.
- Typically presents with anemia or chronic blood loss.
Clinical Presentation and Key Symptoms of Upper GI Bleed
The severity and nature of upper GI bleeding symptoms vary based on the source and volume of blood loss:
- Hematemesis: Vomiting of fresh red blood or coffee-ground material.
- Melena: Black, tarry stools resulting from digested blood.
- Hematochezia: Rare in upper GI bleed unless bleeding is brisk; more typical of lower GI origin.
- Syncope or presyncope: Secondary to hypovolemia.
- Signs of hypovolemic shock: Hypotension, tachycardia, pallor, cold extremities.
- Abdominal pain or discomfort: Localized symptoms based on etiology (e.g., epigastric pain in peptic ulcer).
Diagnostic Approach to Upper GI Hemorrhage
Initial Evaluation
A rapid yet structured assessment is crucial for timely diagnosis:
- History: Focus on NSAID use, alcohol intake, liver disease, vomiting, weight loss.
- Physical Examination: Look for signs of cirrhosis, anemia, or hemodynamic instability.
Laboratory Investigations
- Complete blood count (CBC): Assesses hemoglobin/hematocrit.
- Liver function tests: Evaluate for variceal etiology.
- Coagulation profile: Essential in cirrhosis or anticoagulant use.
- Blood urea nitrogen (BUN)/creatinine ratio: Elevated BUN suggests upper GI origin.
Risk Stratification Tools
- Glasgow-Blatchford Score (GBS): Predicts need for intervention.
- Rockall Score: Assesses mortality risk and rebleed potential.
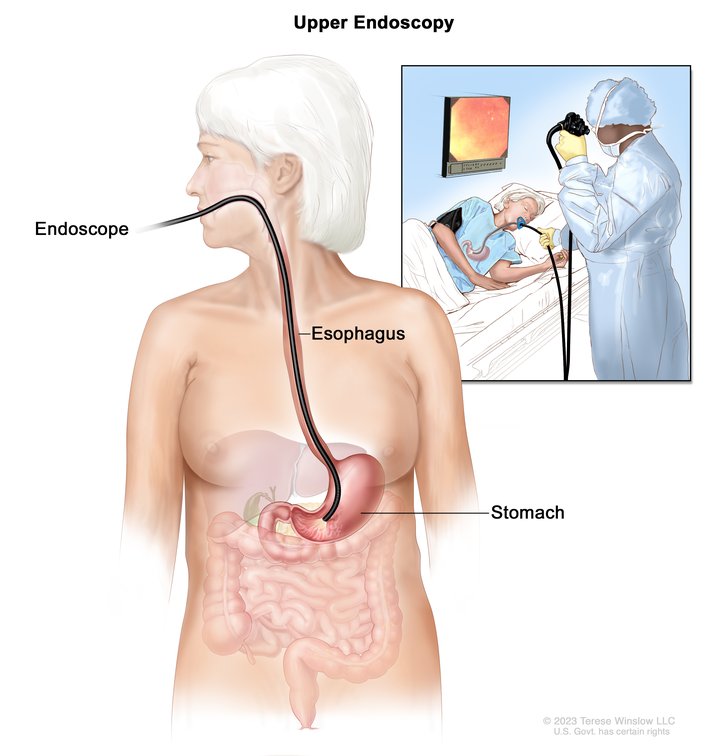
Endoscopic Evaluation
Upper endoscopy (esophagogastroduodenoscopy – EGD) is the gold standard for both diagnosis and treatment. It should be performed within 24 hours of presentation, or emergently in cases of hemodynamic instability.
Treatment and Management of Upper GI Bleed
Resuscitation and Stabilization
- Airway protection in altered sensorium or active hematemesis.
- Two large-bore IV lines for fluid resuscitation.
- Crystalloid infusion followed by type-specific blood transfusion as needed.
- Correct coagulopathy with fresh frozen plasma or platelets.
Pharmacologic Therapy
- Proton Pump Inhibitors (PPIs): High-dose IV therapy (e.g., pantoprazole) to stabilize clots in ulcer bleeding.
- Octreotide: Used in suspected variceal bleeding to reduce portal hypertension.
- Antibiotics: Prophylaxis in cirrhotic patients to prevent spontaneous bacterial peritonitis (SBP).
Endoscopic Therapy
- Thermal coagulation, injection therapy, or clipping for ulcers.
- Band ligation or sclerotherapy for varices.
- Adrenaline injection often used as a first-line hemostatic technique.
Surgical and Radiologic Interventions
- Surgery is indicated when endoscopic therapy fails or in massive, unrelenting hemorrhage.
- Transarterial embolization (TAE) is an alternative for high-risk surgical candidates or inaccessible lesions.
Special Considerations in Upper GI Bleeding
Rebleeding Risk
- High-risk stigmata (e.g., active arterial bleed, visible vessel) require close monitoring and repeat endoscopy.
- Patients with cirrhosis or coagulopathy are more prone to recurrence.
Antithrombotic Agents
- Temporarily withhold anticoagulants until hemostasis is achieved.
- Restart based on individualized risk-benefit assessment post-stabilization.
Post-Endoscopy Care
- Continue PPI infusion for 72 hours in high-risk ulcer bleeds.
- Repeat H. pylori testing and eradication therapy if positive.
- Plan for follow-up endoscopy in selected cases (e.g., malignancy suspicion).
Prognosis and Outcomes
Outcomes depend on bleeding severity, comorbidities, and timeliness of intervention:
- Mortality rate: 3–14% depending on etiology and patient profile.
- Variceal bleeds: Higher mortality and recurrence than peptic ulcers.
- Early endoscopy: Reduces need for transfusion, surgery, and hospital stay.
Patients should be enrolled in long-term follow-up and receive secondary prophylaxis if high-risk (e.g., beta-blockers for varices, maintenance PPIs).
Upper GI bleeding remains a critical gastrointestinal emergency requiring prompt recognition, thorough diagnostic evaluation, and rapid therapeutic intervention. A multidisciplinary approach involving gastroenterology, intensive care, interventional radiology, and surgery ensures optimal patient outcomes. Endoscopic therapy remains the cornerstone of management, supported by pharmacologic and hemodynamic stabilization measures. Prevention of recurrence and comprehensive post-procedural care are essential for long-term success.