Percutaneous Transluminal Coronary Angioplasty (PTCA) is a widely practiced interventional procedure for revascularizing stenosed coronary arteries. However, the occurrence of unstable angina pectoris during PTCA presents a significant clinical challenge, often signaling acute myocardial ischemia, vessel spasm, or procedural complications such as thrombus formation or dissection. Recognizing and managing this phenomenon in real-time is essential for ensuring procedural success and patient safety.
Pathophysiological Mechanisms Behind Angina During PTCA
Unstable angina during PTCA arises due to transient or sustained myocardial ischemia triggered by one or more procedural events:
- Transient occlusion due to balloon inflation
- Distal thromboembolism
- Plaque rupture or dissection
- Abrupt vessel closure
- Microvascular obstruction
- No-reflow phenomenon
These mechanisms acutely reduce myocardial perfusion, resulting in chest pain, ischemic ECG changes, and potential hemodynamic instability.
Clinical Manifestations of Unstable Angina During PTCA
Unstable angina presents acutely and may vary in severity based on the extent of ischemia and patient comorbidities. Common features during angioplasty include:
- Sudden-onset chest discomfort or pain, often retrosternal
- Radiation to neck, jaw, or upper limbs
- ST-segment depression or elevation on real-time ECG monitoring
- Bradycardia or tachycardia
- Hypotension or hypertension
- Ventricular arrhythmias in severe ischemia
Symptom onset typically correlates with balloon inflation, guidewire manipulation, or stent deployment.
Common Causes of Unstable Angina During PTCA
1. Balloon Inflation-Induced Ischemia
Temporary cessation of blood flow during inflation may provoke angina, especially in high-grade stenosis or if collateral circulation is poor.
2. Plaque Rupture and Thrombus Formation
Mechanical disruption of vulnerable plaques may lead to acute thrombus formation, reducing downstream perfusion.
3. Coronary Artery Dissection
Intimal tearing from balloon dilation or stent placement can create a false lumen, resulting in luminal compromise.
4. Distal Embolization
Dislodged atherothrombotic debris may travel distally, causing occlusion in smaller branches and microvascular ischemia.
5. No-Reflow Phenomenon
Despite vessel patency, microcirculatory dysfunction can impair perfusion, particularly in long-standing or thrombotic lesions.
Intra-Procedural Monitoring and Diagnosis
Real-time assessment of angina during PTCA relies on continuous clinical and hemodynamic monitoring.
Electrocardiography (ECG)
- Detects ST-segment changes in real-time.
- Differentiates transient ischemia from evolving infarction.
Hemodynamic Parameters
- Blood pressure and heart rate monitoring help assess the extent of myocardial stress.
- Sudden drops in systolic BP may indicate severe ischemia or left ventricular dysfunction.
Angiographic Findings
- Abrupt vessel closure, dissection flaps, thrombus formation, or impaired flow (TIMI <3) directly visualize pathology.
Immediate Management of Unstable Angina During PTCA
Timely action during an angina episode ensures vessel patency and prevents myocardial infarction.
Pharmacologic Interventions
- Intracoronary nitroglycerin: Relieves spasm and reduces preload.
- Aspirin and P2Y12 inhibitors: Reinforce antiplatelet coverage.
- Unfractionated heparin or bivalirudin: Maintains anticoagulation.
- Glycoprotein IIb/IIIa inhibitors (e.g., abciximab): Indicated in thrombus-heavy lesions or no-reflow states.
- Adenosine or verapamil: Administered intracoronarily for no-reflow.
Mechanical Interventions
- Reinflation of the balloon: May restore flow in dynamic occlusion.
- Stent placement: Seals dissections or ruptured plaques.
- Aspiration thrombectomy: Removes obstructive thrombi.
- Intra-aortic balloon pump (IABP): Used in hemodynamic collapse to support coronary perfusion.
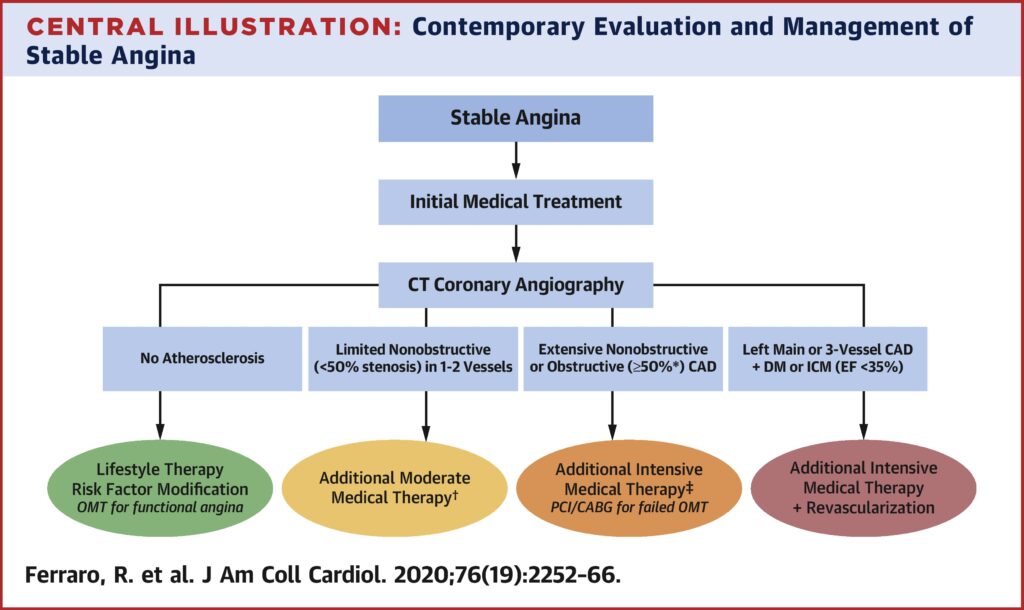
Risk Factors and Patient Profiles Prone to Intra-PTCA Angina
Patients with certain risk factors have increased susceptibility to unstable angina during the procedure:
- Complex lesions: Bifurcation, calcified, or chronic total occlusions
- Multivessel disease
- Diabetes mellitus
- Recent acute coronary syndrome
- High thrombus burden
- Reduced left ventricular ejection fraction
These factors should guide pre-procedural planning and intra-operative vigilance.
Preventive Strategies for Minimizing Angina Risk During PTCA
Pre-Procedural Optimization
- Loading with dual antiplatelets: At least 12–24 hours before elective PTCA
- Statins: Reduce periprocedural inflammation and plaque destabilization
- Intravenous nitroglycerin: Prevents coronary spasm in reactive vessels
Procedural Techniques
- Gentle lesion handling
- Stepwise balloon dilations
- Use of embolic protection devices in saphenous vein graft interventions
- Pre-dilatation and lesion preparation to reduce risk of dissection
Post-Procedural Monitoring and Follow-Up
Even after successful PTCA, patients who experienced unstable angina intra-procedurally should undergo:
- Serial cardiac enzymes (troponin, CK-MB) to assess myocardial injury
- Post-procedural ECGs
- Echocardiography if arrhythmias or hemodynamic abnormalities are observed
- Intensive coronary care monitoring for 24–48 hours
Prognostic Implications and Outcomes
Unstable angina during PTCA is associated with:
- Increased periprocedural myocardial infarction risk
- Higher incidence of in-stent thrombosis
- Greater likelihood of target lesion revascularization (TLR)
- Possible long-term impairment in ventricular function
Timely identification and effective response mitigate these risks and preserve procedural success.
Unstable angina pectoris during PTCA is an acute and high-stakes complication reflecting myocardial ischemia due to dynamic procedural factors. Meticulous technique, real-time monitoring, and swift pharmacologic or mechanical intervention are essential to manage these episodes effectively. With appropriate risk stratification and intra-procedural strategy, the prognosis can be significantly improved, ensuring safer coronary revascularization outcomes.