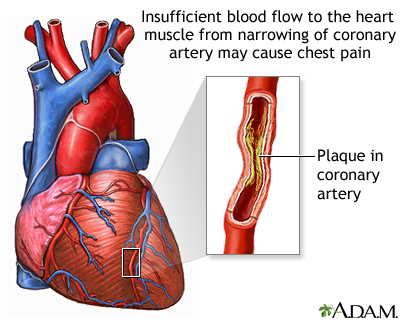
Unstable angina pectoris is a life-threatening condition characterized by unexpected chest pain due to inadequate blood flow to the heart muscle. Unlike stable angina, which occurs predictably with exertion, unstable angina can manifest at rest or with minimal exertion, signifying a high risk of myocardial infarction (heart attack). Prompt identification and management are essential to improving patient outcomes and preventing irreversible cardiac damage.
Understanding the Pathophysiology of Unstable Angina
Unstable angina is most often a consequence of atherosclerotic plaque rupture within the coronary arteries. This rupture exposes thrombogenic substances, leading to platelet aggregation and partial thrombus formation. The result is a critical reduction in coronary blood flow without complete occlusion, distinguishing it from ST-elevation myocardial infarction (STEMI).
Clinical Features and Symptoms of Unstable Angina
Recognition of unstable angina symptoms is crucial for timely intervention. Common clinical features include:
- Chest pain or discomfort at rest or with minimal exertion
- Prolonged angina episodes lasting more than 20 minutes
- New-onset angina classified as severe (Class III by the Canadian Cardiovascular Society)
- Worsening stable angina, with increased frequency or intensity
- Pain radiating to the left arm, jaw, neck, or back
- Associated symptoms: shortness of breath, sweating, nausea, dizziness
Unlike stable angina, unstable angina is unpredictable and may occur without physical exertion.
Risk Factors and Causes of Unstable Angina
Several underlying conditions increase the likelihood of developing unstable angina. These include:
- Atherosclerosis (primary cause)
- Hypertension
- Hyperlipidemia
- Smoking
- Diabetes mellitus
- Family history of coronary artery disease
- Obesity and sedentary lifestyle
Triggers may include acute stress, sudden exertion, cold exposure, or recent illness.
Diagnostic Evaluation of Unstable Angina
Electrocardiogram (ECG)
An ECG is the first-line tool to assess patients presenting with chest pain. In unstable angina:
- ST-segment depression
- T-wave inversions
- No persistent ST-segment elevation
Cardiac Biomarkers
Unstable angina is non-infarctional; hence, troponin and CK-MB levels remain within normal limits, differentiating it from NSTEMI.
Additional Diagnostic Tools
- Echocardiography: to assess left ventricular function
- Stress Testing: typically deferred during acute episodes
- Coronary Angiography: definitive imaging to detect obstructive coronary lesions
- CT Coronary Angiogram: non-invasive alternative in select cases
Risk Stratification and Clinical Scoring
Risk stratification tools guide treatment decisions:
- TIMI Risk Score
- GRACE Risk Score
These tools evaluate:
- Age
- Cardiac biomarker levels
- ECG changes
- Known CAD
- Frequency and severity of angina
- Hemodynamic instability
Immediate Management of Unstable Angina
Prompt treatment is necessary to reduce myocardial oxygen demand and restore perfusion.
Anti-Ischemic Therapy
- Nitroglycerin (sublingual or IV): vasodilation and pain relief
- Beta-blockers: reduce heart rate and myocardial oxygen consumption
- Calcium channel blockers: alternative for beta-blocker intolerance
Antiplatelet Agents
- Aspirin (loading dose): irreversible COX-1 inhibition
- P2Y12 inhibitors (Clopidogrel, Ticagrelor): dual antiplatelet therapy to prevent clot propagation
Anticoagulants
- Unfractionated heparin or low molecular weight heparin (e.g., enoxaparin) to inhibit thrombin generation
Statins
- High-intensity statin therapy is initiated early, regardless of lipid levels, for plaque stabilization.
Revascularization Strategies
Patients at high or intermediate risk benefit from early invasive strategies:
Percutaneous Coronary Intervention (PCI)
- Preferred for patients with accessible lesions
- Involves balloon angioplasty and stent placement
Coronary Artery Bypass Grafting (CABG)
- Indicated in multivessel disease or left main coronary artery involvement
Early revascularization has been shown to improve mortality and reduce recurrent ischemic events.
Long-Term Management and Secondary Prevention
Post-acute care focuses on reducing recurrence and slowing disease progression:
Lifestyle Modifications
- Smoking cessation
- Heart-healthy diet (Mediterranean or DASH diet)
- Regular physical activity
- Weight loss
Pharmacologic Therapy
- Long-term aspirin and P2Y12 inhibitors
- Beta-blockers for at least 3 years
- ACE inhibitors or ARBs for patients with hypertension or diabetes
- Statins for LDL-C control below 70 mg/dL
Monitoring
- Regular cardiovascular follow-up
- Lipid profile, blood pressure, and glycemic control assessment
- Cardiac rehabilitation for functional recovery
Prognosis and Complications
Unstable angina is a precursor to myocardial infarction. Without intervention, approximately 10–20% of patients may progress to infarction within weeks.
Poor Prognostic Indicators
- Persistent chest pain despite therapy
- Elevated heart rate or low systolic blood pressure
- Widespread ST depression on ECG
- Comorbidities (e.g., diabetes, renal failure)
Unstable angina pectoris represents a critical warning sign of impending myocardial infarction. Accurate diagnosis, prompt initiation of anti-ischemic and antithrombotic therapy, and appropriate revascularization are crucial. Long-term secondary prevention strategies must be emphasized to reduce recurrence and improve patient survival. A multidisciplinary approach involving cardiologists, primary care providers, and rehabilitation specialists ensures optimal outcomes in managing this high-risk cardiovascular condition.