Ulcerative proctitis represents a localized form of ulcerative colitis confined to the rectum. Though often considered a milder variant within the spectrum of inflammatory bowel diseases (IBD), ulcerative proctitis demands precise diagnosis and tailored management to prevent disease progression and optimize patient outcomes. This article provides an in-depth analysis of ulcerative proctitis, detailing its clinical presentation, diagnostic procedures, therapeutic interventions, and long-term management, ensuring a robust foundation for healthcare providers and patients alike.
Understanding Ulcerative Proctitis: Definition and Pathophysiology
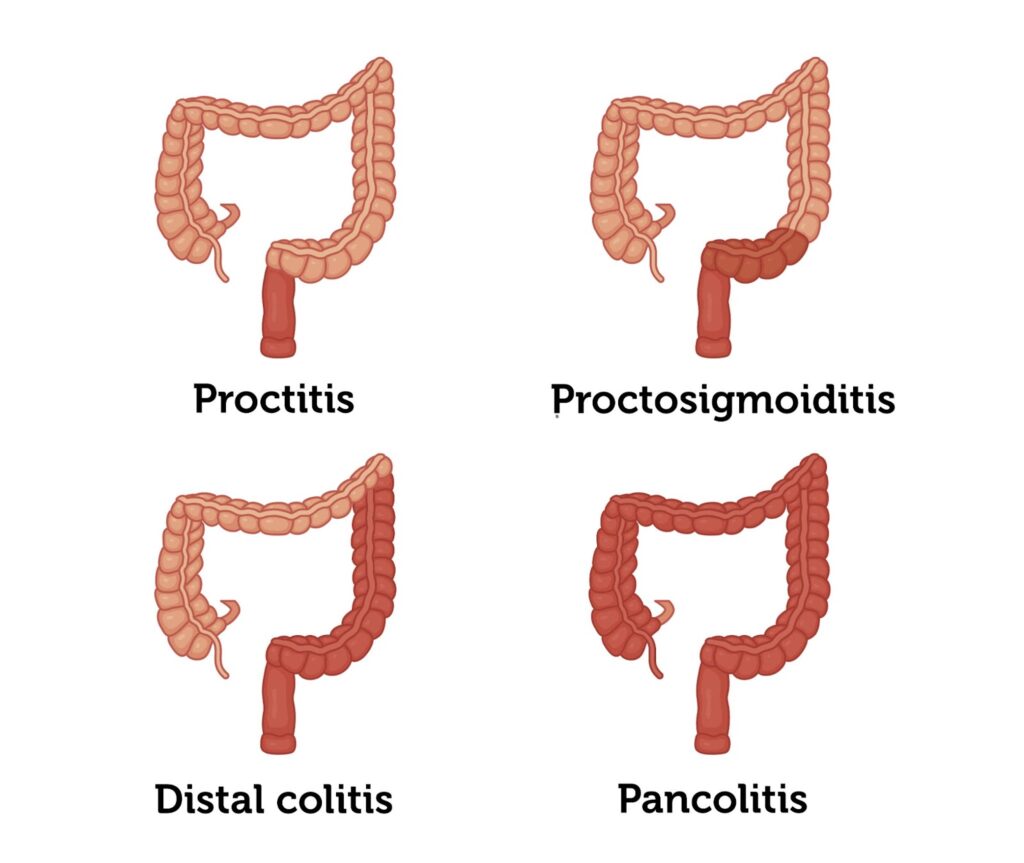
Ulcerative proctitis is an inflammatory condition limited to the rectal mucosa, characterized by continuous inflammation beginning at the anal verge and extending proximally up to 15 cm. Unlike more extensive forms of ulcerative colitis, proctitis does not involve the colon beyond the rectum, yet it can cause significant morbidity through persistent rectal symptoms.
The pathophysiology involves an aberrant immune response targeting the rectal mucosa, resulting in epithelial damage, ulceration, and infiltration by inflammatory cells. Genetic predisposition, environmental triggers, and microbiome alterations contribute to disease onset and activity.
Clinical Presentation: Recognizing Ulcerative Proctitis Symptoms
Ulcerative proctitis typically manifests with:
- Rectal bleeding: The most common symptom, often presenting as bright red blood mixed with stool.
- Tenesmus: A persistent sensation of incomplete evacuation.
- Rectal urgency and frequency: Patients may experience frequent bowel movements, sometimes accompanied by mucus discharge.
- Mild to moderate abdominal discomfort: Primarily localized to the rectal area.
Symptom severity can fluctuate, with periods of exacerbation and remission. Importantly, systemic symptoms such as fever and weight loss are uncommon, differentiating proctitis from more extensive colitis.
Diagnostic Approach: Confirming Ulcerative Proctitis
Accurate diagnosis hinges on a combination of clinical evaluation, endoscopic visualization, histopathological assessment, and exclusion of infectious etiologies.
Endoscopy
Flexible sigmoidoscopy is the preferred initial diagnostic tool, revealing erythema, friability, ulcerations, and loss of vascular pattern localized to the rectum.
Biopsy and Histology
Histological examination confirms chronic inflammation with crypt architectural distortion, crypt abscesses, and mucosal ulceration, hallmark features of ulcerative proctitis.
Laboratory Tests
- Stool studies exclude infections such as Clostridioides difficile.
- Inflammatory markers including fecal calprotectin and C-reactive protein assist in assessing disease activity.
Treatment Options for Ulcerative Proctitis: Induction and Maintenance of Remission
Treatment goals focus on symptom relief, mucosal healing, and prevention of disease progression.
First-Line Therapies
- Topical 5-Aminosalicylic Acid (5-ASA): Rectal suppositories or enemas deliver high local drug concentrations with minimal systemic absorption, effectively inducing remission.
- Oral 5-ASA agents: Used adjunctively, especially when inflammation extends beyond the rectum.
Corticosteroids
- Topical corticosteroids: Such as hydrocortisone or budesonide enemas are reserved for patients unresponsive to 5-ASA therapy.
- Systemic corticosteroids: Rarely required but indicated for severe or refractory disease.
Advanced Therapeutics
In cases of persistent or severe proctitis, immunomodulators (azathioprine) and biologics (anti-TNF agents like infliximab) may be warranted.
Managing Ulcerative Proctitis: Long-Term Strategies and Monitoring
Long-term management aims to maintain remission and monitor for complications.
- Maintenance therapy: Continuation of topical or oral 5-ASA is standard to prevent relapse.
- Regular follow-up: Clinical assessment and occasional endoscopy monitor disease status.
- Patient education: Emphasizing adherence and recognition of relapse signs.
Potential Complications and Disease Progression
Though ulcerative proctitis generally carries a favorable prognosis, vigilance is essential as up to 30% of patients may experience proximal extension of inflammation into the sigmoid colon or beyond, evolving into left-sided or extensive colitis. Persistent inflammation increases risks for strictures, bleeding, and colorectal neoplasia, necessitating periodic surveillance.
Lifestyle and Dietary Considerations in Ulcerative Proctitis Management
While no specific diet cures proctitis, certain nutritional and lifestyle adjustments mitigate symptom severity:
- Avoiding irritants such as caffeine, alcohol, and spicy foods.
- Maintaining adequate hydration and balanced nutrition.
- Managing stress through behavioral therapies as psychological factors can exacerbate symptoms.
Ulcerative proctitis, though localized, requires prompt recognition and strategic management to alleviate symptoms and avert progression. Through targeted topical therapies, vigilant monitoring, and supportive lifestyle adjustments, we can achieve sustained remission and improve patient quality of life. Early intervention and ongoing care remain paramount in mitigating long-term risks associated with this condition.