Ulcerative colitis (UC) is a chronic inflammatory condition of the colon and rectum that falls under the umbrella of inflammatory bowel disease (IBD). It significantly impacts quality of life and requires long-term management. This article provides an authoritative and medically accurate overview of ulcerative colitis, including its etiology, clinical manifestations, diagnostic criteria, therapeutic strategies, and lifestyle modifications.
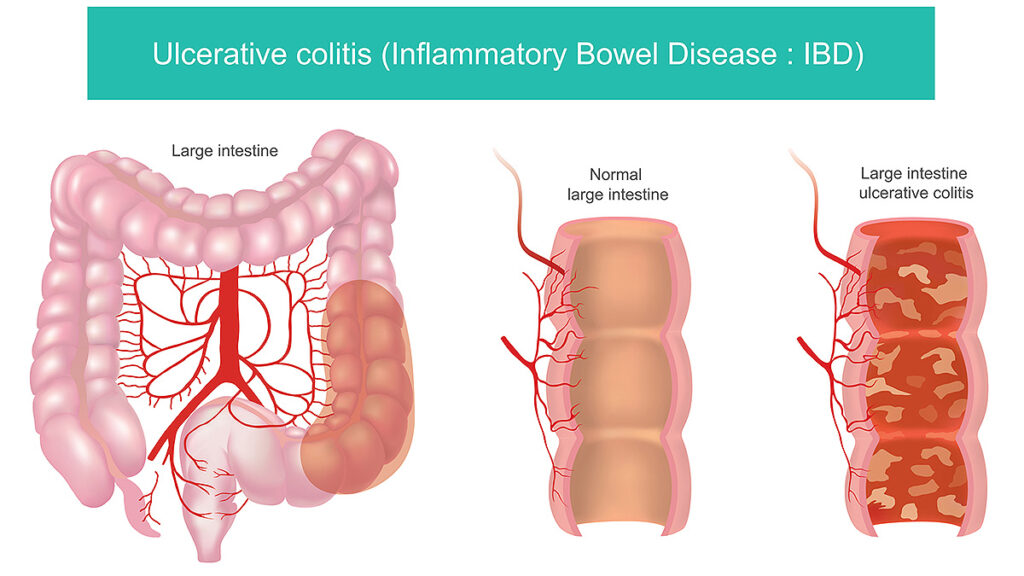
Understanding Ulcerative Colitis: Definition and Pathophysiology
Ulcerative colitis is characterized by continuous mucosal inflammation starting from the rectum and extending proximally in the colon. Unlike Crohn’s disease, which can affect any part of the gastrointestinal tract and all layers of the bowel wall, UC is restricted to the colonic mucosa.
Pathogenesis
UC results from an inappropriate immune response to intestinal microbiota in genetically susceptible individuals. A compromised epithelial barrier allows antigens to penetrate, triggering a cascade of cytokine-mediated inflammation.
Key Causes and Risk Factors of Ulcerative Colitis
Although the exact cause remains unknown, several risk factors contribute to the onset and progression of UC:
- Genetics: Family history increases the risk, particularly among first-degree relatives.
- Immune system dysfunction: Autoimmune processes lead to self-directed inflammation.
- Environmental influences: Western diet, pollution, and urban living conditions are correlated.
- Gut microbiome imbalances: Dysbiosis may initiate or exacerbate colonic inflammation.
- NSAIDs and antibiotics: These may alter the intestinal lining and gut flora, potentially triggering disease onset.
Common Signs and Symptoms of Ulcerative Colitis
Ulcerative colitis presents with episodic flare-ups and periods of remission. The clinical spectrum ranges from mild discomfort to life-threatening complications.
Major Symptoms
- Persistent diarrhea, often with blood or mucus
- Abdominal pain and cramping, typically in the lower left quadrant
- Urgency and tenesmus (sensation of incomplete evacuation)
- Rectal bleeding
- Fatigue and weight loss
Systemic and Extraintestinal Manifestations
- Fever during flares
- Anemia due to chronic blood loss
- Arthritis
- Erythema nodosum and pyoderma gangrenosum (skin lesions)
- Uveitis and episcleritis (eye inflammation)
- Primary sclerosing cholangitis (liver complication)
Disease Classification by Extent and Severity
Ulcerative colitis is classified based on the location and intensity of inflammation:
| Classification | Area Affected | Symptoms Severity |
|---|---|---|
| Ulcerative Proctitis | Rectum only | Mild, limited bowel frequency |
| Left-sided Colitis | Rectum to splenic flexure | Moderate pain, bloody stool |
| Pancolitis | Entire colon | Severe symptoms, systemic effects |
Diagnostic Approach to Ulcerative Colitis
Prompt and accurate diagnosis is essential to guide treatment and monitor disease activity.
Diagnostic Methods
- Colonoscopy with biopsy: Confirms diagnosis; shows continuous mucosal inflammation, ulceration, and pseudopolyps.
- Stool studies: Rule out infectious causes (e.g., C. difficile, Salmonella).
- Blood tests: Elevated C-reactive protein (CRP), anemia, leukocytosis.
- Fecal calprotectin: Marker of intestinal inflammation, helpful in monitoring response to treatment.
- Imaging: CT or MRI may assess complications like toxic megacolon.
Medical Treatment Options for Ulcerative Colitis
The goal of therapy is to induce and maintain remission, prevent complications, and improve quality of life. Treatment is stratified based on disease severity and extent.
First-Line Therapies
- 5-Aminosalicylic Acid (5-ASA):
- Mesalamine is effective for mild-to-moderate disease.
- Administered orally or rectally depending on inflammation location.
Corticosteroids
- Used for moderate to severe flares.
- Prednisone and budesonide reduce inflammation but are not suitable for long-term use due to adverse effects.
Immunomodulators
- Azathioprine and 6-mercaptopurine: For steroid-dependent or refractory cases.
- Require regular blood monitoring due to potential myelosuppression.
Biologic Therapies
- Anti-TNF agents: Infliximab, adalimumab.
- Anti-integrin therapy: Vedolizumab (gut-selective).
- Anti-IL-12/23: Ustekinumab for moderate-to-severe UC.
JAK Inhibitors
- Tofacitinib: Oral small molecule, approved for moderate-to-severe UC.
- Rapid onset but associated with infection risk.
Surgical Management and Indications
Surgery may become necessary in the following scenarios:
- Fulminant colitis or toxic megacolon
- Dysplasia or colorectal cancer
- Intractable symptoms despite maximal medical therapy
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) remains the standard surgical approach, offering cure from colitis but requiring lifestyle adaptation.
Ulcerative Colitis Diet and Nutritional Strategies
No single diet cures UC, but nutritional modifications help control symptoms and reduce flare frequency.
Recommended Practices
- Low-residue diet during flares to reduce bowel volume.
- High-calorie, high-protein diet to combat weight loss.
- Lactose restriction in those with secondary intolerance.
Foods to Avoid
- Alcohol, caffeine, spicy foods
- Raw vegetables, nuts, seeds during active flares
- High-fat, ultra-processed foods
Working with a registered dietitian is advised for personalized guidance.
Living with Ulcerative Colitis: Lifestyle and Mental Health
Chronic illness impacts mental well-being and daily functioning. Effective management includes:
- Stress reduction: Mindfulness, therapy, yoga, and support groups.
- Medication adherence: Prevents relapses and complications.
- Regular screenings: Colonoscopy surveillance for cancer risk every 1–2 years after 8–10 years of disease.
Ulcerative Colitis in Children and Adolescents
Pediatric UC presents more extensively and aggressively than in adults. Growth delay and psychosocial impact are major concerns. Early initiation of advanced therapies and nutritional support is critical for optimal outcomes.
Prognosis and Long-Term Outlook
Most individuals with UC can achieve remission with proper management. However, lifelong monitoring is necessary due to:
- Risk of colorectal cancer (especially with pancolitis >10 years)
- Medication side effects
- Cumulative impact on daily life and work productivity
Early diagnosis, personalized treatment, and comprehensive care improve long-term health outcomes.
FAQs
What causes ulcerative colitis?
The exact cause is unknown, but genetic predisposition, immune dysregulation, and environmental factors contribute.
Can ulcerative colitis be cured?
There is no medical cure, but surgery (proctocolectomy) can eliminate the disease. Medications manage symptoms and maintain remission.
Is ulcerative colitis life-threatening?
While not typically fatal, severe flares or complications like toxic megacolon can be life-threatening without proper treatment.
What foods worsen ulcerative colitis?
High-fiber foods, dairy, spicy items, alcohol, and ultra-processed products may aggravate symptoms during flares.
How is ulcerative colitis different from Crohn’s disease?
UC affects only the colon and rectal mucosa in a continuous pattern, while Crohn’s can affect any part of the GI tract in patchy segments and full-thickness inflammation.