Typhoid fever, a life-threatening systemic illness, remains a significant public health challenge, particularly in regions with poor sanitation and limited access to clean water. Caused by the bacterium Salmonella enterica serotype Typhi (S. Typhi), the disease is transmitted primarily through the ingestion of contaminated food or water. A coordinated approach encompassing early detection, prompt treatment, and preventive strategies is essential to controlling its spread.
Understanding the Pathogen: Salmonella Typhi
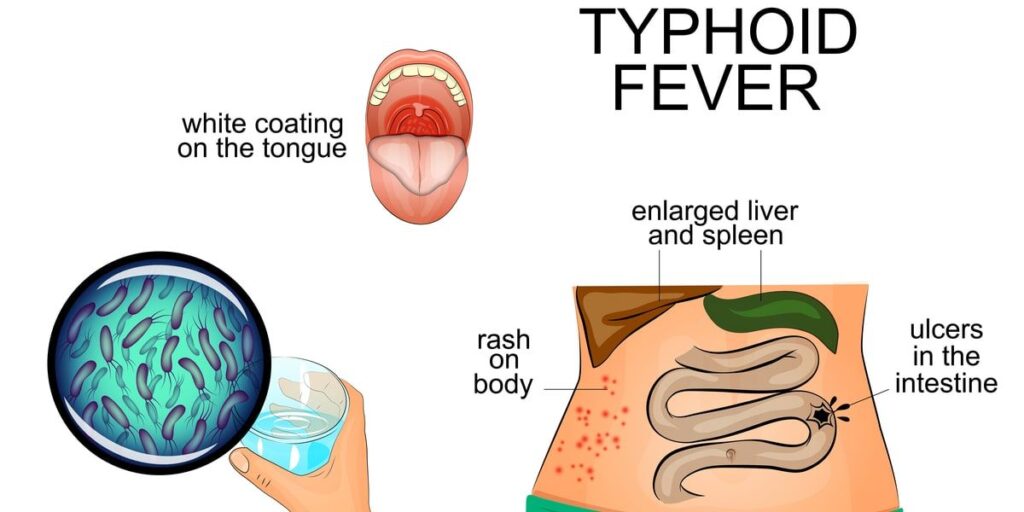
Salmonella Typhi is a gram-negative, motile bacillus belonging to the Enterobacteriaceae family. It is strictly a human pathogen with no animal reservoir. Once ingested, S. Typhi crosses the intestinal epithelium, invades macrophages, and disseminates via the bloodstream to infect the liver, spleen, and bone marrow.
Transmission Routes and Risk Factors
Typhoid fever spreads predominantly via the fecal-oral route. Risk factors include:
- Consumption of food or water contaminated with feces from infected individuals
- Poor hand hygiene
- Inadequate sanitation infrastructure
- Travel to endemic regions
- Close contact with chronic carriers
Clinical Manifestations of Typhoid Fever
Symptoms usually begin 6 to 30 days after exposure. The illness progresses through distinct stages if left untreated:
Early Stage (Week 1)
- Gradual onset of sustained fever
- Fatigue and malaise
- Headache
- Dry cough
- Abdominal discomfort
Advanced Stage (Week 2–3)
- High-grade fever (up to 104°F / 40°C)
- Rose-colored spots on the trunk
- Hepatosplenomegaly
- Abdominal distension
- Diarrhea or constipation
- Delirium (referred to as “typhoid state”)
Complications (Week 3–4)
- Intestinal perforation
- Gastrointestinal bleeding
- Encephalopathy
- Sepsis and shock
Without treatment, mortality rates can reach up to 20%.
Diagnosis: Confirming Typhoid Fever
Early and accurate diagnosis is critical to effective management. Diagnostic methods include:
1. Blood Culture
- Gold standard in the first week of illness
- Sensitivity decreases over time
2. Bone Marrow Culture
- Most sensitive (even after antibiotic use)
- Invasive but highly specific
3. Stool and Urine Culture
- Useful in later stages of illness
- Aids in detecting chronic carriers
4. Widal Test
- Detects antibodies against S. Typhi antigens
- Prone to false positives in endemic areas
5. Rapid Diagnostic Tests (RDTs)
- Provide quick results
- Include TUBEX and Typhidot
Treatment Strategies for Typhoid Fever
First-Line Antibiotics
- Ceftriaxone (IV/IM): Broad-spectrum and effective for severe cases
- Azithromycin: Preferred in uncomplicated infections
- Ciprofloxacin: Effective in regions with low resistance
Drug Resistance Concerns
The rise of multidrug-resistant (MDR) and extensively drug-resistant (XDR) S. Typhi has complicated treatment protocols. Resistance to chloramphenicol, ampicillin, and trimethoprim-sulfamethoxazole is widespread in certain areas.
Alternative Treatments:
- Meropenem and tigecycline for XDR cases
- Combination therapy for complicated infections
Supportive Care
- Adequate hydration
- Antipyretics
- Nutritional support
Prevention: Protecting Against Typhoid Fever
1. Vaccination
Two vaccines are currently in use:
- Ty21a (oral): Live-attenuated; 4-dose regimen; not for immunocompromised
- Vi polysaccharide (injectable): Single-dose; booster every 2–3 years
WHO recommends routine immunization in endemic areas.
2. Sanitation and Hygiene
- Use of safe drinking water
- Proper handwashing with soap
- Adequate sewage disposal
- Safe food handling practices
3. Travel Precautions
- Avoid raw fruits and vegetables unless peeled
- Drink bottled or boiled water
- Eat food that is thoroughly cooked and served hot
Chronic Carriage and Public Health Implications
Approximately 1–5% of infected individuals become chronic carriers, shedding bacteria in stool or urine for over a year. These carriers, often asymptomatic, serve as a continuous source of infection, necessitating strict public health monitoring.
Key actions include:
- Screening food handlers
- Long-term antibiotic therapy for carriers
- Public education and awareness campaigns
Global Burden and Epidemiology
- Estimated 11–21 million cases annually
- Over 100,000 deaths worldwide each year
- Highest prevalence in South Asia, sub-Saharan Africa, and parts of Southeast Asia
Vaccination campaigns, clean water initiatives, and antibiotic stewardship programs have shown promise in reducing incidence rates.
Typhoid fever remains a significant global health concern, especially in areas with poor sanitation and limited healthcare access. A multipronged approach—combining early diagnosis, effective antibiotic therapy, vaccination, and improved hygiene—forms the cornerstone of control and prevention. With rising antibiotic resistance, global collaboration in surveillance, vaccine coverage, and public health infrastructure is essential for long-term eradication of this preventable disease.

