The management of type 2 diabetes mellitus (T2DM) has evolved beyond simple glycemic control. Adjunctive therapies play a crucial role in addressing the multifactorial nature of the disease by improving metabolic outcomes, reducing complications, and enhancing patient quality of life. The optimal use of these adjuncts requires a strategic integration of pharmacological agents, lifestyle interventions, and advanced monitoring tools.
The Role of Adjunct Therapy in T2DM Management
Adjunctive treatment in T2DM refers to additional therapeutic measures used alongside first-line agents such as metformin. The purpose is to improve glycemic control, mitigate cardiovascular risks, promote weight loss, and slow disease progression.
Key benefits of adjunct therapies include:
- Enhanced insulin sensitivity
- Cardiovascular and renal protection
- Weight reduction
- Beta-cell preservation
- Reduction in medication-related adverse effects
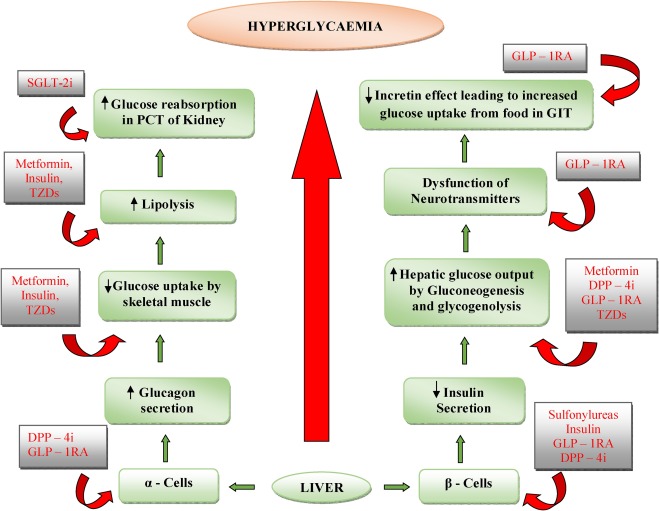
Pharmacological Adjuncts: Classes and Mechanisms
GLP-1 Receptor Agonists: A Dual Benefit Approach
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) enhance glucose-dependent insulin secretion and suppress glucagon release, while also delaying gastric emptying and reducing appetite.
Examples:
- Liraglutide
- Semaglutide
- Dulaglutide
Benefits:
- Significant HbA1c reduction (~1.0–1.5%)
- Weight loss (2–5 kg)
- Reduced major cardiovascular events
GLP-1 RAs are ideal adjuncts for overweight or obese patients with high cardiovascular risk.
SGLT2 Inhibitors: Renal and Cardiac Synergy
Sodium-glucose co-transporter 2 inhibitors reduce renal glucose reabsorption, leading to glycosuria and caloric loss.
Examples:
- Empagliflozin
- Dapagliflozin
- Canagliflozin
Clinical Benefits:
- Moderate HbA1c lowering
- Cardiovascular event reduction
- Slower progression of diabetic nephropathy
- Lowered blood pressure
SGLT2 inhibitors are strongly recommended in patients with established cardiovascular disease, heart failure, or chronic kidney disease.
Lifestyle-Based Adjunct Strategies
Medical Nutrition Therapy (MNT)
A personalized eating plan by a registered dietitian supports sustained glycemic control.
Core Components:
- Low glycemic index carbohydrates
- Adequate fiber intake
- Caloric restriction for overweight patients
- Mediterranean or DASH-style patterns
MNT has been shown to reduce HbA1c by 0.3–1.0% depending on adherence and dietary modifications.
Physical Activity Enhancement
Routine exercise improves insulin sensitivity, promotes weight loss, and reduces cardiovascular risk.
Recommendations:
- ≥150 minutes/week of moderate-intensity aerobic activity
- Resistance training ≥2 days/week
- Reduce sedentary time
Behavioral Therapy
Cognitive-behavioral strategies and motivational interviewing are effective in fostering long-term adherence to therapeutic regimens.
Insulin Therapy as an Adjunct in T2DM
When oral agents and non-insulin injectables fail to maintain target glycemia, insulin is introduced as an adjunct.
Basal Insulin
Initiated with long-acting agents such as glargine or degludec to control fasting plasma glucose.
Intensification Options
- Basal-bolus regimen: For comprehensive glycemic control
- Premixed insulin: For simplified administration in selected patients
Insulin as adjunct is particularly beneficial in cases of:
- Severe hyperglycemia (HbA1c >10%)
- Marked symptomatic presentation
- Beta-cell failure
Adjunctive Use of Incretin Combinations
Emerging therapies combine multiple hormone pathways to amplify benefits.
GLP-1 + GIP Dual Agonists
Tirzepatide, a dual GLP-1/GIP receptor agonist, shows superior glycemic and weight-loss outcomes versus standalone GLP-1 analogs.
Advantages:
- HbA1c reductions >2.0%
- Up to 10–15% body weight loss
- Cardiometabolic improvement
Nutraceuticals and Complementary Agents
While not substitutes for standard care, certain evidence-based supplements may act as safe adjuncts:
- Berberine: Improves insulin sensitivity
- Alpha-lipoic acid: Reduces neuropathic pain and oxidative stress
- Vitamin D: May support glycemic control in deficient individuals
- Omega-3 fatty acids: Cardioprotective in hypertriglyceridemic patients
These agents should be used cautiously and in consultation with a healthcare provider.
Digital Health Tools as Adjunctive Aids
Continuous Glucose Monitoring (CGM)
CGM devices provide real-time glucose data, improve time-in-range, and help refine therapy adjustments.
Benefits:
- Greater HbA1c reduction compared to SMBG
- Fewer hypoglycemia episodes
- Enhanced patient engagement
Mobile Apps and Telemedicine
Digital platforms offering medication reminders, lifestyle tracking, and virtual consultations serve as valuable adjuncts in chronic care management.
Individualizing Adjunct Therapy in Clinical Practice
Adjunctive treatments should be tailored based on:
- Patient phenotype (obese, lean, insulin-deficient)
- Comorbidities (CVD, CKD, heart failure)
- Glycemic targets and prior therapy response
- Patient preference and adherence capability
A holistic, patient-centric strategy enables durable metabolic control and long-term risk reduction.
Adjunctive treatment strategies for type 2 diabetes mellitus are essential components of modern diabetes care. Through the integration of pharmacological agents like GLP-1 receptor agonists and SGLT2 inhibitors, structured lifestyle modifications, insulin therapy when needed, and innovative technologies, we can achieve superior glycemic control, reduce complications, and elevate the standard of patient care. Proper selection and sequencing of these adjuncts, based on individual risk profiles and therapeutic goals, are key to optimizing outcomes in T2DM management.